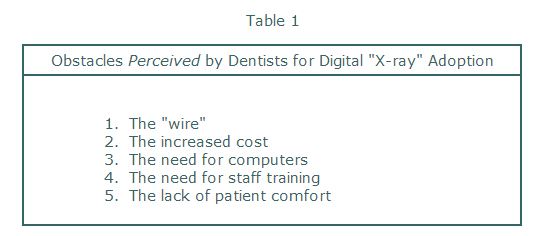
I will address several of these perceived obstacles in combination.
The "wire" and Patient Comfort
In my opinion, the only valid objection to using a sensor with a wire comes from the pediatric dentist or general dentist treating many children in their practice. And this is only with patients (read kids) under 5 or 6 years old. Two, three and four year-olds just don't get it. Tell them to close and they bite. Tell them to bite and they chew. The fiber optic cables of wired sensors may not live up to the abuse. However, for the rest of the dentists patient population, the solid-state systems can work exceptionally well - even for the gaggers!
Placing a sensor is more comfortable than placing intraoral film! Yes, you heard right. How many films have dentists and their staff bent to place "more comfortably" in the mouth. How many patients have complained about the film "cutting" their gums. We've all had these experiences. And yet, at least one phosphor manufacturer, to gain a competitive marketing advantage, claims that the phosphor plates are "as comfortable as film". WAKE UP AND SMELL THE FIXER! FILM HAS NEVER BEEN ALL THAT COMFORTABLE.
With a good paralleling instrument, with proper receptor placement, with appropriate training (or in some cases, retraining), a hard plastic, wired sensor is MORE comfortable than film or phosphor plates. I know this because I have participants of my "Digital 'Re-boot' Camp" place all three receptors. They are all very surprised that the sensor, placed away from the arch (working out on the end of the biteblock) is far more comfortable than film or phosphor. And, for those people considering phosphor plates, YOU CAN'T BEND THE PLATE! In fact, the plates take as much "care and feeding" as the solid-state detectors. Sure they're digital, but they're not without drawbacks (later).
So what about the gaggers? A person that has a BAD gag reflex is an operator problem. And sometimes our techniques to overcome the gagging, techniques taught to us by instructors in recognized programs, are just wrong. If I ask an audience "What's the first thing to you tell the patient to do to help them stop?", the answer is most commonly "Breath through your nose". WRONG!
Breathing through the nose with the mouth partially open on a biteblock is impossible for most people. Try it yourself. Open your mouth about 25 mm and place 2 fingers between your bicuspids. Then try breathing through your nose. Your soft palate elevates, closes off the airway and you can't get air. When the patient's trying this, they hold their breath, can't get air, and think they're going to die! That's what causes the gagging.
Try telling them to breath through their mouth when it's open. It's more natural, they get air, they usually do not gag. You can demonstrate this to them , with them and instruct them to "keep breathing through your mouth" during the image acquisition. It works! I know, because I've used it for 25 years.
So the point is that receptor placement with a sensor is more comfortable with adult patients. It just takes a good technique. The wire comes out of the mouth along the PID bar and can even be clipped to the metal bar in some systems.
Increased Cost and Need for Computers
This is really a "perceived" problem. Dentists and lab owners look only at the initial "capital investment". Sure the systems appear costly. The sensors are costly to make. But the ROI (return on investment in this case, not region of interest) is realized in less than 1 year in most cases. In December, 1999 in the Journal of the California Dental Association, we published the comparison between a film-based and digital system - both initial and "on-going" costs2. The digital systems won "hands down". You can see this article on my web site www.learndigital.net. More recently I addressed how I feel EIP (Electronic Image Processing) will enhance the dentist's "bottom line"3.
Sure the dentist or laboratory owner has to have computers in the office/lab. These days, most do. For the dentist, digital x-ray adoption means moving computers into the clinical areas. This does add cost. But, computer costs have come down dramatically, displays are more ergonomic, glass front, flat panel screens are even disinfectable (see Figure 2 later). Dentists do "educate" their patients, chairside, and those who have adopted these systems find them indispensable. These are only a few reasons to "Go Digital". I've published a more complete list elsewhere recently4.
Finally, the "mark-up" on a radiographic service is huge. The ROI on radiographic procedures is probably the highest of anything done in the office. I'm sure that radiographic lab owners know this already. It's my colleagues that are slow to grasp this concept.
The Need for Staff Training
My dentist colleagues and even manufacturers are finally grasping the reality that training is probably the most critical need for successful digital technology adoption. Proper training is required for both dentist and staff.
The staff must perfect excellent image acquisition skills. The dentist must acquire and practice good electronic image processing skills.
Notice that in Table 1 I did not list the perceived problem of the "dentist's image processing skills". Frankly, most dentists don't realize they need this training to successfully use their new technology. This is a part of the slow adoption problem. That is that DENTISTS DON'T DO THE IMAGE ACQUISITION!
For all these years, dentists have delegated the image acquisition to the staff member. Many of these staff members were trained by the dentists themselves. Most of these staff members thus learned "Bisecting-the-Angle" (BA) technique as their primary tool for performing x-ray procedures.BISECTING-THE-ANGLE TECHNIQUE DOES NOT WORK WELL WITH SOLID-STATE DETECTORS.
This being said, I do not believe that the majority my colleagues actually undertake any new procedure in their offices without obtaining proper training for both themselves and their staff. But the real problem in my opinion with dentists adopting digital "x-ray" imaging systems is that the dentist doesn't DO the technique. Air abrasion units, lasers, electric handpieces, caries detection tools like the DiagnodentTM are used in the dentist's hands. If they had to do the image acquisition, I think they would flock to the use of solid-state "x-ray" detectors.
Real Obstacles
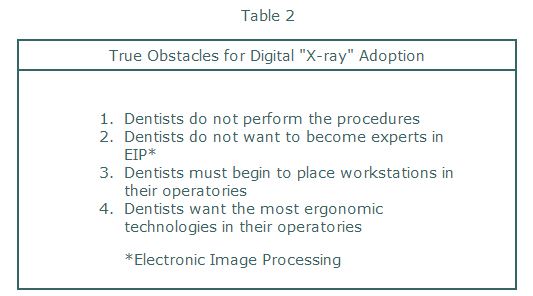
It is obvious from the preceding discussion that the biggest real obstacle to dentists adopting these systems is that they don't perform the radiographic procedures, but rather delegate them. Table 2 below outlines what I feel are the true or real obstacles to digital "x-ray" adoption.
The "wire" and Patient Comfort
In my opinion, the only valid objection to using a sensor with a wire comes from the pediatric dentist or general dentist treating many children in their practice. And this is only with patients (read kids) under 5 or 6 years old. Two, three and four year-olds just don't get it. Tell them to close and they bite. Tell them to bite and they chew. The fiber optic cables of wired sensors may not live up to the abuse. However, for the rest of the dentists patient population, the solid-state systems can work exceptionally well - even for the gaggers!
Placing a sensor is more comfortable than placing intraoral film! Yes, you heard right. How many films have dentists and their staff bent to place "more comfortably" in the mouth. How many patients have complained about the film "cutting" their gums. We've all had these experiences. And yet, at least one phosphor manufacturer, to gain a competitive marketing advantage, claims that the phosphor plates are "as comfortable as film". WAKE UP AND SMELL THE FIXER! FILM HAS NEVER BEEN ALL THAT COMFORTABLE.
With a good paralleling instrument, with proper receptor placement, with appropriate training (or in some cases, retraining), a hard plastic, wired sensor is MORE comfortable than film or phosphor plates. I know this because I have participants of my "Digital 'Re-boot' Camp" place all three receptors. They are all very surprised that the sensor, placed away from the arch (working out on the end of the biteblock) is far more comfortable than film or phosphor. And, for those people considering phosphor plates, YOU CAN'T BEND THE PLATE! In fact, the plates take as much "care and feeding" as the solid-state detectors. Sure they're digital, but they're not without drawbacks (later).
So what about the gaggers? A person that has a BAD gag reflex is an operator problem. And sometimes our techniques to overcome the gagging, techniques taught to us by instructors in recognized programs, are just wrong. If I ask an audience "What's the first thing to you tell the patient to do to help them stop?", the answer is most commonly "Breath through your nose". WRONG!
Breathing through the nose with the mouth partially open on a biteblock is impossible for most people. Try it yourself. Open your mouth about 25 mm and place 2 fingers between your bicuspids. Then try breathing through your nose. Your soft palate elevates, closes off the airway and you can't get air. When the patient's trying this, they hold their breath, can't get air, and think they're going to die! That's what causes the gagging.
Try telling them to breath through their mouth when it's open. It's more natural, they get air, they usually do not gag. You can demonstrate this to them , with them and instruct them to "keep breathing through your mouth" during the image acquisition. It works! I know, because I've used it for 25 years.
So the point is that receptor placement with a sensor is more comfortable with adult patients. It just takes a good technique. The wire comes out of the mouth along the PID bar and can even be clipped to the metal bar in some systems.
Increased Cost and Need for Computers
This is really a "perceived" problem. Dentists and lab owners look only at the initial "capital investment". Sure the systems appear costly. The sensors are costly to make. But the ROI (return on investment in this case, not region of interest) is realized in less than 1 year in most cases. In December, 1999 in the Journal of the California Dental Association, we published the comparison between a film-based and digital system - both initial and "on-going" costs2. The digital systems won "hands down". You can see this article on my web site www.learndigital.net. More recently I addressed how I feel EIP (Electronic Image Processing) will enhance the dentist's "bottom line"3.
Sure the dentist or laboratory owner has to have computers in the office/lab. These days, most do. For the dentist, digital x-ray adoption means moving computers into the clinical areas. This does add cost. But, computer costs have come down dramatically, displays are more ergonomic, glass front, flat panel screens are even disinfectable (see Figure 2 later). Dentists do "educate" their patients, chairside, and those who have adopted these systems find them indispensable. These are only a few reasons to "Go Digital". I've published a more complete list elsewhere recently4.
Finally, the "mark-up" on a radiographic service is huge. The ROI on radiographic procedures is probably the highest of anything done in the office. I'm sure that radiographic lab owners know this already. It's my colleagues that are slow to grasp this concept.
The Need for Staff Training
My dentist colleagues and even manufacturers are finally grasping the reality that training is probably the most critical need for successful digital technology adoption. Proper training is required for both dentist and staff.
The staff must perfect excellent image acquisition skills. The dentist must acquire and practice good electronic image processing skills.
Notice that in Table 1 I did not list the perceived problem of the "dentist's image processing skills". Frankly, most dentists don't realize they need this training to successfully use their new technology. This is a part of the slow adoption problem. That is that DENTISTS DON'T DO THE IMAGE ACQUISITION!
For all these years, dentists have delegated the image acquisition to the staff member. Many of these staff members were trained by the dentists themselves. Most of these staff members thus learned "Bisecting-the-Angle" (BA) technique as their primary tool for performing x-ray procedures.BISECTING-THE-ANGLE TECHNIQUE DOES NOT WORK WELL WITH SOLID-STATE DETECTORS.
This being said, I do not believe that the majority my colleagues actually undertake any new procedure in their offices without obtaining proper training for both themselves and their staff. But the real problem in my opinion with dentists adopting digital "x-ray" imaging systems is that the dentist doesn't DO the technique. Air abrasion units, lasers, electric handpieces, caries detection tools like the DiagnodentTM are used in the dentist's hands. If they had to do the image acquisition, I think they would flock to the use of solid-state "x-ray" detectors.
Real Obstacles
It is obvious from the preceding discussion that the biggest real obstacle to dentists adopting these systems is that they don't perform the radiographic procedures, but rather delegate them. Table 2 below outlines what I feel are the true or real obstacles to digital "x-ray" adoption.
Electronic Image Processing
Unfortunately, for dentists, they MUST acquire some elementary skills in Electronic Image Processing or EIP. EIP is the most important reason for adopting digital radiographic technology. The ability to perform feature extraction for tasks such as carious lesion detection, periodontal bone loss and periapical lesion assessment are improved tremendously by the digital systems. Dentistry is finally doing what medicine has done for 20 years or more. Dentists can now change the image characteristics to make better clinical decisions.
In order to help dentists make this transition more easily, some manufacturers have begun to write software programs (called algorithms) to enhance the image characteristics for a specific task like caries detection. Carious lesions are best seen with high contrast images. Planmeca Corporation has introduced a software program called "Quasimor" which has 3 "tools" for optimizing the image characteristics for caries, periodontal bone evaluation and periapical lesion assessment. None of these tools are yet "expert" systems; that is, none actually find the lesions for the clinician. But, they represent the first step in simplifying the dentist's tasks and helping the dentist with the detection of problems so he/she can provide better patient care. Figure 1 shows the "Quasimor" interface.
Unfortunately, for dentists, they MUST acquire some elementary skills in Electronic Image Processing or EIP. EIP is the most important reason for adopting digital radiographic technology. The ability to perform feature extraction for tasks such as carious lesion detection, periodontal bone loss and periapical lesion assessment are improved tremendously by the digital systems. Dentistry is finally doing what medicine has done for 20 years or more. Dentists can now change the image characteristics to make better clinical decisions.
In order to help dentists make this transition more easily, some manufacturers have begun to write software programs (called algorithms) to enhance the image characteristics for a specific task like caries detection. Carious lesions are best seen with high contrast images. Planmeca Corporation has introduced a software program called "Quasimor" which has 3 "tools" for optimizing the image characteristics for caries, periodontal bone evaluation and periapical lesion assessment. None of these tools are yet "expert" systems; that is, none actually find the lesions for the clinician. But, they represent the first step in simplifying the dentist's tasks and helping the dentist with the detection of problems so he/she can provide better patient care. Figure 1 shows the "Quasimor" interface.
Operatory Workstations
Slowly, though not quite so slow as digital "x-ray" adoption, dentists are moving computers into the operatory. In March 2002, Gail Wesimann of Dental Products Report published results of a "technology" survey revealing what the next technology purchases were likely to be for dental offices5. The list includes, in order of interest:
Slowly, though not quite so slow as digital "x-ray" adoption, dentists are moving computers into the operatory. In March 2002, Gail Wesimann of Dental Products Report published results of a "technology" survey revealing what the next technology purchases were likely to be for dental offices5. The list includes, in order of interest:
- Digital radiography system (wired sensor) 43%
- Digital still camera 43%
- LCD flat panel monitor 38%
- Telescopic loupes 32%
- High speed Internet connection 28%
Ergonomic Technologies
Clutter in the dental office, especially in the operatory, is not good. Many "technology" items that dentists have or are considering purchasing do occupy significant space. This probably explains, in part, the interest in flat panel displays. Laser systems, air abrasion units, digital x-ray systems some video camera systems, patient education systems?most of these technologies have cart delivery systems. There is only so much space in the operatory!
My vision of ergonomic technology for the radiographic procedures we perform in dental offices, radiographic labs, hospitals and orthopedic clinics is a portable, lightweight x-ray generator, for a variety of tasks, preferably "hand-held". Ok, I know this will sound like a "sales pitch", but I have patented and manufactured 5 working prototypes of just such a device.
Think of it: no x-ray generator mounted on the wall, no need to plan a dental (or radiographic) operatory around the x-ray unit, quicker image acquisition, no retakes (because we fix the receptor - film, phosphor, or CCD/CMOS - to the x-ray device), easily transported into the OR or to a patient's room on a hospital floor, and no need to add another cart in the operatory. This would be a product, I believe, that would hasten the transition to digital "x-ray" systems in dentistry. The operator benefits, the RT benefits, the auxiliary benefits and the patient benefits. A presentation about the unit will be par of my talk at the next AADMRT meeting in Las Vegas.
Clutter in the dental office, especially in the operatory, is not good. Many "technology" items that dentists have or are considering purchasing do occupy significant space. This probably explains, in part, the interest in flat panel displays. Laser systems, air abrasion units, digital x-ray systems some video camera systems, patient education systems?most of these technologies have cart delivery systems. There is only so much space in the operatory!
My vision of ergonomic technology for the radiographic procedures we perform in dental offices, radiographic labs, hospitals and orthopedic clinics is a portable, lightweight x-ray generator, for a variety of tasks, preferably "hand-held". Ok, I know this will sound like a "sales pitch", but I have patented and manufactured 5 working prototypes of just such a device.
Think of it: no x-ray generator mounted on the wall, no need to plan a dental (or radiographic) operatory around the x-ray unit, quicker image acquisition, no retakes (because we fix the receptor - film, phosphor, or CCD/CMOS - to the x-ray device), easily transported into the OR or to a patient's room on a hospital floor, and no need to add another cart in the operatory. This would be a product, I believe, that would hasten the transition to digital "x-ray" systems in dentistry. The operator benefits, the RT benefits, the auxiliary benefits and the patient benefits. A presentation about the unit will be par of my talk at the next AADMRT meeting in Las Vegas.
What's Next?
I have described the future of software innovation for intraoral digital radiography. The development of algorithms that are task specific will have a very positive impact on dentists considering purchase of a solid-state or phosphor x-ray system. I actually believe that the first digital x-ray system dentists might purchase will be a panoramic one. I have outlined this in an upcoming article, for the publication Dental Economics6. Believe it or not, I think that the ROI on a digital panoramic system is even quicker than with an intraoral system. And, the "learning curve" is much quicker for the auxiliary. And, "patient comfort" is almost a non-issue with panoramic image acquisition. And, there's no gagging. And, the doctor can learn the same EIP techniques he/she needs for intraoral image processing. And, the future software will probably lend itself to 3D representation of problems like bone loss, canal structure, etc...
And, I could go on!
Summary
So, we've seen manufacturers begin to address the problems of simplifying image processing tools. We've seen that more ergonomic technology is on the way. We've seen that dentists are indeed employing computers more commonly in their operatories. So what's left?
I truly believe that the biggest challenge we all have, those of us who want dentistry to catch up to the commercial world and medical community, is the challenge to train auxiliaries, dentists, and yes, even sales representatives to understand and employ proper image acquisition using digital sensors/receptors and proper electronic image processing techniques to extract the most useful information from these images to improve patient management. If I didn't believe this, I'd still be resisting the transition to digital instead of embracing and championing it! And, I hope this information has convinced you to "Go Digital"!
I have described the future of software innovation for intraoral digital radiography. The development of algorithms that are task specific will have a very positive impact on dentists considering purchase of a solid-state or phosphor x-ray system. I actually believe that the first digital x-ray system dentists might purchase will be a panoramic one. I have outlined this in an upcoming article, for the publication Dental Economics6. Believe it or not, I think that the ROI on a digital panoramic system is even quicker than with an intraoral system. And, the "learning curve" is much quicker for the auxiliary. And, "patient comfort" is almost a non-issue with panoramic image acquisition. And, there's no gagging. And, the doctor can learn the same EIP techniques he/she needs for intraoral image processing. And, the future software will probably lend itself to 3D representation of problems like bone loss, canal structure, etc...
And, I could go on!
Summary
So, we've seen manufacturers begin to address the problems of simplifying image processing tools. We've seen that more ergonomic technology is on the way. We've seen that dentists are indeed employing computers more commonly in their operatories. So what's left?
I truly believe that the biggest challenge we all have, those of us who want dentistry to catch up to the commercial world and medical community, is the challenge to train auxiliaries, dentists, and yes, even sales representatives to understand and employ proper image acquisition using digital sensors/receptors and proper electronic image processing techniques to extract the most useful information from these images to improve patient management. If I didn't believe this, I'd still be resisting the transition to digital instead of embracing and championing it! And, I hope this information has convinced you to "Go Digital"!
REFERENCES
- Hatcher DC: NewTom 9000, Currents Summer: 1, 16-17, 2002.
- Miles DA, Langlais RP and Parks ET: Digital x-rays are here; why aren't you using them? J California Dent Assoc. 27(12): 926-934, 1999.
- Miles DA: Get Ready to "Go Digital", Dental Economics May, 2002, pp. 72-76.
- Miles DA: Choosing a Digital X-ray System, Dental Equipment and Materials May, 2002, pp. 25-27.
- Weisman, G: 2002 Technology Census: A survey report Dental Products Report, June 2002.
- Miles DA: Digital Panoramic Imaging - Could It Be My First Digital X-ray System, Dental Economics, 2002 (in press).