To date, many practitioners, specialists and generalists alike, are still limiting their dental implants' diagnosis and treatment planning to evaluation of study casts, anesthetizing and probing the depth of the mucosa over the bone, and the use of panoramic and or lateral skull radiographs. The later two are frequently used to determine the appropriateness of the alveolar bone and its relationship to critical anatomical landmarks.
In the same time, over the past couple of decades, a large number of peered reviewed professional manuscripts documented that optimal and critical implant size and orientation can be significantly aided by a cross-sectional, three-dimensional radiographic exam. Some even strongly advocated computed tomography (CT) as the appropriate pre-operative diagnostic modality prior to implant placement(10-35).
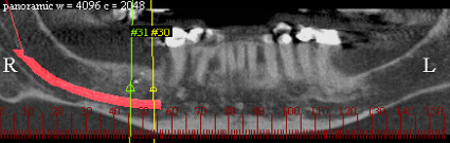
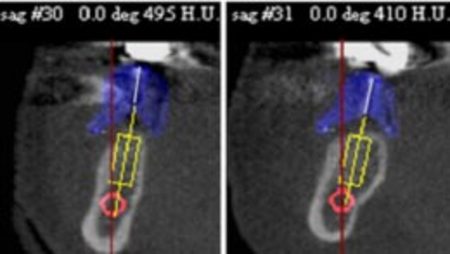
Moreover, the complementary use of radiographic guides, designed based on restorative principles, along with cross sectional imaging, was proclaimed to further advance diagnosis and treatment planning.(36-39) The use of cross sectional imaging reveals the outline, width and height of the bone, and relationship to anatomical landmarks. The addition of radiographic surgical guides, provides a precise illustration of the bone-to-implant and bone-to-planned prosthetic trajectory correlation. Different types of radiographic guides have been introduced to market over the years, all consisting of a radiopaque markers, suggestive of the planned prosthetic trajectory (PPT). Patients wear the radiographic guides during the cross-sectional exam. Information obtained from the imaging phase is then transferred to both the surgical and restorative phases of treatment (Figure 1).
In the same time, over the past couple of decades, a large number of peered reviewed professional manuscripts documented that optimal and critical implant size and orientation can be significantly aided by a cross-sectional, three-dimensional radiographic exam. Some even strongly advocated computed tomography (CT) as the appropriate pre-operative diagnostic modality prior to implant placement(10-35).
Moreover, the complementary use of radiographic guides, designed based on restorative principles, along with cross sectional imaging, was proclaimed to further advance diagnosis and treatment planning.(36-39) The use of cross sectional imaging reveals the outline, width and height of the bone, and relationship to anatomical landmarks. The addition of radiographic surgical guides, provides a precise illustration of the bone-to-implant and bone-to-planned prosthetic trajectory correlation. Different types of radiographic guides have been introduced to market over the years, all consisting of a radiopaque markers, suggestive of the planned prosthetic trajectory (PPT). Patients wear the radiographic guides during the cross-sectional exam. Information obtained from the imaging phase is then transferred to both the surgical and restorative phases of treatment (Figure 1).
The Future of Oral Implantology
In a recent report from Kalorama Information,(7) a complete analysis of the growing dental implant market worldwide is provided. It is estimated that growth in implant-based dental reconstruction products will outstrip other areas of dental devices and products. According to the report, in the industrial world, over 240 million people lack one or more teeth. It is estimated that 40% of the western population is missing at least one tooth. In the United States, roughly 10% of the population is edentulous, and every year approximately two million Americans loose one or more teeth due to sporting accidents.
Additionally, the Kalorama report states that replacing a tooth with the traditional fixed partial bridges (FPB), which consists of a pontic that is attached to two surrounding crowns (abutments), has been shown to be problematic, and newer more permanent solutions are needed.
According to the Kalorama report, one of the most important developments in modern dentistry has been permanent tooth replacement with dental implants. Also, bone grafting and regeneration techniques have expanded the possibilities for implant-based restorative dentistry. These techniques are making it possible to enlarge the candidate pool for implants to include a sizable population who were poor candidates for dental implantation due to severe bone resorption.
What's more, the Kalorama report asserts that with the rapidly aging population trend in the developed world, a large number of companies see the opportunity to move into these sophisticated dental techniques.
In addition, a number of renowned professionals have cautioned our profession not to place a fixed partial bridge (FPB) between "virgin" teeth, that is, unless the patient refused the option of a dental implant, otherwise, the case might end up in court. According to Gordon Christensen if adequate bone is present, implants are state-of-the-art for everything from a single missing tooth to an edentulous case, and in order to serve the American public well and in adequate capacity, many more practitioners should make the effort to become proficient in this area.(40)
Yet, according to another renowned professional like Morton Perel,(41) universal proficiency in the field of oral implantology is lacking. Many implants are misplaced either in poor angulations (48%) and/or distribution (29%). Ironically, and rightfully so, Morton Perel compares placing implants to throwing darts.
How can we Assure more Predictable and Successful Outcomes
As discussed earlier, the use of advanced cross sectional imaging technologies in conjunction with radiographic guides has long been advocated to further enhance the scope of the pre-operative diagnostic information.(10-39) Moreover, in the mid 90s, utilizing different assessment methodologies, two manuscripts(42, 43) forecasted the future of imaging technologies in oral implantology, including the notion of a CT-based surgical guidance system was anticipated the in the 90s (Figures 2-4).
In a recent report from Kalorama Information,(7) a complete analysis of the growing dental implant market worldwide is provided. It is estimated that growth in implant-based dental reconstruction products will outstrip other areas of dental devices and products. According to the report, in the industrial world, over 240 million people lack one or more teeth. It is estimated that 40% of the western population is missing at least one tooth. In the United States, roughly 10% of the population is edentulous, and every year approximately two million Americans loose one or more teeth due to sporting accidents.
Additionally, the Kalorama report states that replacing a tooth with the traditional fixed partial bridges (FPB), which consists of a pontic that is attached to two surrounding crowns (abutments), has been shown to be problematic, and newer more permanent solutions are needed.
According to the Kalorama report, one of the most important developments in modern dentistry has been permanent tooth replacement with dental implants. Also, bone grafting and regeneration techniques have expanded the possibilities for implant-based restorative dentistry. These techniques are making it possible to enlarge the candidate pool for implants to include a sizable population who were poor candidates for dental implantation due to severe bone resorption.
What's more, the Kalorama report asserts that with the rapidly aging population trend in the developed world, a large number of companies see the opportunity to move into these sophisticated dental techniques.
In addition, a number of renowned professionals have cautioned our profession not to place a fixed partial bridge (FPB) between "virgin" teeth, that is, unless the patient refused the option of a dental implant, otherwise, the case might end up in court. According to Gordon Christensen if adequate bone is present, implants are state-of-the-art for everything from a single missing tooth to an edentulous case, and in order to serve the American public well and in adequate capacity, many more practitioners should make the effort to become proficient in this area.(40)
Yet, according to another renowned professional like Morton Perel,(41) universal proficiency in the field of oral implantology is lacking. Many implants are misplaced either in poor angulations (48%) and/or distribution (29%). Ironically, and rightfully so, Morton Perel compares placing implants to throwing darts.
How can we Assure more Predictable and Successful Outcomes
As discussed earlier, the use of advanced cross sectional imaging technologies in conjunction with radiographic guides has long been advocated to further enhance the scope of the pre-operative diagnostic information.(10-39) Moreover, in the mid 90s, utilizing different assessment methodologies, two manuscripts(42, 43) forecasted the future of imaging technologies in oral implantology, including the notion of a CT-based surgical guidance system was anticipated the in the 90s (Figures 2-4).

Figure 4: Utilizing ImplantMasterTM (I-Dent, Ltd. Hod Hasharon, Israel), a 3-D reconstruction of a patient's anatomy was achieved and a surgical guidance template was designed and e-mailed for computer Rapid Manufacturing with precise drilling holes' distribution and trajectory, in which stainless steal sleeves with the prescribed inner diameter are glued in.
The notion of these methodologies generated an intense professional debate. Shortly after the AAOMR position paper(44) on preoperative implant site assessment was published, many challenged its validity. In a follow-up editorial, Brooks(45) asked the question: "Where's the evidence?" Does CT imaging in the preoperative stage of dental implants have any value, or is it simply another relatively expensive test that has no effect on the outcome in the majority of cases? Other questions raised in the editorial were whether the experience level of the clinician makes a difference in what type of imaging is necessary, does the amount of bone determined clinically make a difference and are there alternative methods to obtain information about undercuts and bone inclination that work better and are less expensive?
A year later, the American Academy of Oral and Maxillofacial Radiology, ad hoc Committee on Parameters of Care, issued an official report regarding parameters of radiologic care, including imaging of dental implant sites.(46) This report stated that panoramic imaging alone is not sufficient for imaging of dental implant sites whereas tomography, either conventional or computed, does provide the necessary radiographic information such as height, density and width of bone.
This report was also followed with a challenging letter to the editor.(47) Shortly after, a rebuttal(48) from the Academy of Oral and Maxillofacial Radiology, ad hoc Committee on Parameters of Care came out, explaining that the Academy's position is one of caution and is derived from adverse effects described in the literature.
Over the years, numerous reports and preliminary clinical studies documented clinical complications with implants and implant prostheses.(49-51) Also, a recent Meta Analysis(52) reported extensively on such complications. In addition, a textbook chapter(53) discusses different implant radiology modalities, their relative strengths and weaknesses, and supplementary imaging guides that might be helpful.
Similarly, the concept of using CT-based dental imaging, coupled with surgical guidance templates is gradually becoming evidence-based through review of recent preliminary clinical studies and case reports.(54-62) These studies describe interactive imaging programs that allow CT studies to be used for planning and constructing a surgical guidance device or navigate the delivery of dental implants at the time of implant placement. The objectives of these preliminary studies were to assess the accuracy of CT-image-based dental implants' planning and surgery. The authors of these studies concluded that these technologies demonstrate progress in oral implantology. However, only one study demonstrated correlating evidence to imaging technology. It showed that the use of conventional cross-sectional tomography before installation of single tooth implants increased the efficacy of periapical plus panoramic images, with respect to the prediction of appropriate implant size, by a factor of 2.5.(63)
Conclusions
Given the recent report from Kalorama Information,(7) the introduction of numerous associated commercial CT-based imaging and surgical guidance platforms and the projected increase in the number of practitioners involved in implant surgery, our profession is bound to go through major changes that will have major effects on the way we view and practice oral implantology. This alone provides sufficient argument for those currently providing services in oral implantology to get gear-up and involved.
While the researchers studying these CT-based imaging and surgical guidance platforms' methodologies agree that more outcomes assessment research has a long term value, in the meantime we must work together to optimize our patient's health.(64)
Many of the authors referenced in this report strongly believe that because dental implants are becoming widespread, careful examination of this pre-operative assessment phase may provide more predictable and successful outcomes, yielding substantial public health benefits. Benefits include preservation of adjacent teeth, lower costs and improved function, to name a few. The impetus to my argument in favor of these new technologies comes from a desire to improve patient care and clinical outcomes. This is a point that many of my colleagues and I have labored over and remain frustrated that our proclamations to this effect are frequently ignored and or present a frequent challenge in dentistry.
A year later, the American Academy of Oral and Maxillofacial Radiology, ad hoc Committee on Parameters of Care, issued an official report regarding parameters of radiologic care, including imaging of dental implant sites.(46) This report stated that panoramic imaging alone is not sufficient for imaging of dental implant sites whereas tomography, either conventional or computed, does provide the necessary radiographic information such as height, density and width of bone.
This report was also followed with a challenging letter to the editor.(47) Shortly after, a rebuttal(48) from the Academy of Oral and Maxillofacial Radiology, ad hoc Committee on Parameters of Care came out, explaining that the Academy's position is one of caution and is derived from adverse effects described in the literature.
Over the years, numerous reports and preliminary clinical studies documented clinical complications with implants and implant prostheses.(49-51) Also, a recent Meta Analysis(52) reported extensively on such complications. In addition, a textbook chapter(53) discusses different implant radiology modalities, their relative strengths and weaknesses, and supplementary imaging guides that might be helpful.
Similarly, the concept of using CT-based dental imaging, coupled with surgical guidance templates is gradually becoming evidence-based through review of recent preliminary clinical studies and case reports.(54-62) These studies describe interactive imaging programs that allow CT studies to be used for planning and constructing a surgical guidance device or navigate the delivery of dental implants at the time of implant placement. The objectives of these preliminary studies were to assess the accuracy of CT-image-based dental implants' planning and surgery. The authors of these studies concluded that these technologies demonstrate progress in oral implantology. However, only one study demonstrated correlating evidence to imaging technology. It showed that the use of conventional cross-sectional tomography before installation of single tooth implants increased the efficacy of periapical plus panoramic images, with respect to the prediction of appropriate implant size, by a factor of 2.5.(63)
Conclusions
Given the recent report from Kalorama Information,(7) the introduction of numerous associated commercial CT-based imaging and surgical guidance platforms and the projected increase in the number of practitioners involved in implant surgery, our profession is bound to go through major changes that will have major effects on the way we view and practice oral implantology. This alone provides sufficient argument for those currently providing services in oral implantology to get gear-up and involved.
While the researchers studying these CT-based imaging and surgical guidance platforms' methodologies agree that more outcomes assessment research has a long term value, in the meantime we must work together to optimize our patient's health.(64)
Many of the authors referenced in this report strongly believe that because dental implants are becoming widespread, careful examination of this pre-operative assessment phase may provide more predictable and successful outcomes, yielding substantial public health benefits. Benefits include preservation of adjacent teeth, lower costs and improved function, to name a few. The impetus to my argument in favor of these new technologies comes from a desire to improve patient care and clinical outcomes. This is a point that many of my colleagues and I have labored over and remain frustrated that our proclamations to this effect are frequently ignored and or present a frequent challenge in dentistry.
References
- Adell R, Lekholm U, Rockier B, Branemark PI. A 15-year study of osseointegrated implants in the treatment of the edentulous jaw. Int J Oral Surg 1981;l0:387-4I6.
- James RA, Lozada JL, Truitt PH, Foust BE, Jovanovic SA. Subperiosteal implants. CDAJ 1988:16:10-4.
- Schnitman PA, Shulman LB, editors. NIH-Harvard Consensus Development Conference. Dental implants: Benefit and risk. HHS Summaries. DHHS (NIH) 81-1531, Dec 1980.
- Smithloff M, Fritz ME. The use of blade implants in a selected population of partially edentulous patients: A ten year report. J Periodontol 1982:53:413-8.
- Albrektsson T, Zarb G, Worthington P, Eriksson AR. The long term efficacy of currently used dental implants: A review and proposed criteria of success. Int J Oral Maxillofac Implants 1986;1:11-25.
- Branemark PI, Hansson BO, Adell R, Breine U, Lindstrom J, et al. Osseointegrated implants in the treatment of the edentulous jaw. Experience from a 10-year period. Scand J Plast Reconstr Surg Suppl 1977:16:1-132.
- Kalorama Information, A Division of MarketResearch.com, September 2005. http://www.kaloramainformation.com/pub/1099235.html.
- Tydall DA, Brooks SL. Selection criteria for dental implant site imaging: A position paper of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000;89:630-7.
- Pietrokovski J. The bony residual ridge in man. J Prosthet Dent 1975;34:456-62.
- Clark DE, Danforth RA, Barnes RW, Burtch ML. Radiation absorbed from dental implant radiography: A comparison of linear tomography, CT scan, and panoramic and intra-oral techniques. J Oral Implantol 1990;16:156-64.
- Grondahl K, Ekestubbe A, Grondahl HG, Johnsson T. Reliability of hypocycloidal tomography for the evaluation of the distance from the alveolar crest to the mandibular canal. Dentomaxillofac Radiol 1991;20:200-4.
- Petersson A, Lindh C, Carlsson LE. Estimation of the possibility to treat the edentulous maxilla with osseointegrated implants. Swed Dent J 1992;16:1-6.
- Fredholm U, Bolin A, Andersson L. Pre-implant radiographic assessment of available maxillary bone support: Comparison of tomographic and panoramic technique. Swed Dent J 1993;17:103-9.
- Weinberg LA. CT scan as a radiologic data base for optimum implant orientation. J Prosthet Dent 1993;69:381-5.
- Lam EW, Ruprecht A, Yang J. Comparison of two-dimensional orthoradially. reformatted computed tomography and panoramic radiography for dental implant treatment planning. J Prosthet Dent 1995;74:42-6.
- Lindh C. Radiography of the mandible prior to endosseous implant treatment. Localization of the mandibular canal and assessment of trabecular bone. Swed Dent J 1996;Supp 112:1-45.
- Strid KG. Radiographic procedures. In: Branemark PI, Zarb GA, Albrektsson T, editors. Tissue-integrated prostheses. Osseointegration in clinical dentistry. Chicago: Quintessence, 1985.
- Femandes RJ. Azarbal M, Ismail YH, Curtin HD. A cephalometric tomographic technique to visualize the buccolingual and vertical dimensions of the mandible. J Prosthet Dent 1987;58:466-70.
- Petrikowski CG, Pharoah MJ, Schmitt A. Presurgical radiographic assessment for implants. J Prosthet Dent 1989;61:59-64.
- Stella JP, Tharanon W. A precise radiographic method to determine the location of the inferior alveolar canal in the posterior edentulous mandible: Implications for dental implants. Part 1: Technique. Int J Oral Maxillofac Implants 1990;5:15-22.
- Kassebaum DK, Nummikoski PV, Triplett RO, Langlais RP Cross-sectional radiography for implant site assessment. Oral Surg Oral Med Oral Pathol 1990;70:674-8.
- Eckerdal 0, Kvint S. Pre-surgical planning for osseointegrated implants in the maxilla. A tomographic evaluation of available alveolar bone and morphological relations in the maxilla. Int J Oral Maxillofac Surg 1986:15:722-6.
- Engelman MJ, Sorenson JA, Moy P. Optimum placement of osseointegrated implants. J Prosthet Dent 1988;59:467-73.
- McGivney OP, Haughton V, Strandt JA, Eichholz JE, Lubar DM. A comparison of computer-assisted tomography and data-gathering modalities in prosthodontics. Int J Oral Maxillofac Implants 1986; 1:55-68.
- Rothman SLG, Chaftez N, Rhodes ML, Schwartz MS. CT in the pre-operative assessment of the mandible and maxilla for endosseous implant surgery. Work in progress. Radiology 1988;168:171-5.
- Quirynen M, Lamoral Y, Dedeyser C, Peene P, van Steenburghe D, Bonte J, et al. CT scan standard reconstruction technique for reliable jaw bone volume determination. Int J Oral Maxillofac Implants 1990;5:384-9.
- Abrahams JJ. CT assessment of dental implant planning. Oral Maxillofac Surg Clin North Am 1992;4:1-18.
- Quirynen M, Naert I, van Steenberghe D, Terrlinck J, Dekeyser C, Theuniers G. Periodontal aspects of osseointegrated fixtures supporting an overdenture. A 4-year retrospective study. J Clin Periodontol 1991;18:719-28.
- Jeffcoat M, Jeffcoat RL, Reddy MS, Berland L. Planning interactive implant treatment with 3-D computed tomography. J Am Dent Assoc 1991;122:40-4.
- Tal H, Moses 0. A comparison of panoramic radiography and computed tomography in the planning of implant surgery. Dentomaxillofac Radiol 1991;20:40-2.
- Wishan MS, Bahat 0, Krane M. Computed tomography as an adjunct in dental implant surgery. Int J Periodont Rest Dent 1988;8:30-47,
- Casselman JW, Quirynen M, Lemahieu SF, Baert AL, Bonie J. Computed tomography in the determination of anatomical land-marks in the perspective of endosseous implant installation. J Head Neck Pathol 1988;7:255-64.
- Abrahams JJ, Levine BP. Expanded applications of DentaScan (multiplanar computerized tomography of the mandible and maxilla). Int J Periodont Rest Dent 1990;10:464-71.
- Schwarz MS, Rothman SLG, Rhodes ML, Chafetz N. Computed tomography: Part I. Pre-operative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants 1987;2:137-41.
- Schwarz MS, Rothman SLG, Rhodes ML, Chafetz N. Computed tomography: Part II. Pre-operative assessment of the mandible for endosseous implant surgery. Int J Oral Maxillofac Implants 1987;2:143-48.
- Almog DM, Onufrak JM, Hebel K, Meitner SW. Comparison between planned prosthetic trajectory and residual bone trajectory using surgical guides and tomography: A pilot study. J Oral Implantol 1995;21:275-80.
- Almog DM, Sanchez R. Correlation between planned prosthetic and residual bone trajectories in dental implants. J Prosthet Dent 1999;81:562-7.
- Almog DM, Torrado E, Meitner SW. Fabrication of imaging and surgical guides for dental implants. J Prosthet Dent 2001; 85(5): 504-8.
- Almog DM, Torrado E, Meitner SW, Moss ME, LaMar F. Use of imaging guides in pre-implant tomography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2002;93:483-7.
- Christensen GJ. New Directions in Dentistry. Dentistry Today. 2006 Feb; 108-15.
- Perel ML. Throwing darts. Implant Dent. Editorial 2003;12(4):267.
- Frederiksen NL. Diagnostic imaging in dental implantology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80:540-554.
- Almog DM, Heisler EM. Computer intuition: guiding scientific research in imaging and oral implantology. J Dent Res. 1997;76(10):1684-1689.
- Tyndall AA, Brooks SL. Selection criteria for dental implant site imaging: a position paper of the American Academy of Oral and Maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):630-637.
- Brooks SL. Where's the evidence? (editorial) Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2000;89(5):531.
- White SC. Heslop EW. Hollender LG. Mosier KM. Ruprecht A. Shrout MK. American Academy of Oral and Maxillofacial Radiology, ad hoc Committee on Parameters of Care. Parameters of radiologic care: An official report of the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;91(5):498-511.
- Larson PE. Oral and maxillofacial radiology parameters of care (letter to the editor). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(5):480.
- White SC, Benson BW. Oral and maxillofacial radiology parameters of care (letter to the editor - response). Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(5):480-481.
- Mordenfeld A, Andersson L, Bergstrom B. Hemorrhage in the floor of the mouth during implant placement in the edentulous mandible: a case report. Int J Oral Maxillofac Implants. 1997;12:558-561.
- Givol N, Chaushu G, Halamish-Shani T, Taicher S. Emergency tracheostomy following life-threatening hemorrhage in the floor of the mouth during immediate implant placement in the mandibular canine region. J Periodontol. 2000;71:1893-1895.
- Tepper G, Hofschneider UBH, Gahleitner A, Ulm C. Computer tomographic diagnosis and localization of bone canals in the mandibular interforaminal region for prevention of bleeding complication during implant surgery. Int J Oral Maxillofac Implants. 2001;16:68-72.
- Goodacre CJ, Bernal G, Rungcharassaeng K, Kan JY. Clinical complications with implants and implant prostheses. J Prosthet Dent. 2003;90(2):121-132.
- Shetty V, Benson BW. Orofacial implants. In White SC, Pharoah MJ. Oral Radiology - principles and practice (5th ed). Mosby: Saint Louis. 2004:677-692.
- Siessegger M, Schneider BT, Mischkowski RA, Lazar F, Krug B, Klesper B, Zoller JE. Use of an image-guided navigation system in dental implant surgery in anatomically complex operation sites. J Craniomaxillofac Surg. 2001;29(5):276-281.
- Cavalcanti MG, Ruprecht A, Vannier MW. 3D volume rendering using multislice CT for dental implants. Dentomaxillofac Radiol. 2002;31(4):218-223.
- Fortin T, Champleboux G, Bianchi S, Buatois H, Coudert JL.Precision of transfer of preoperative planning for oral implants based on cone-beam CT-scan images through a robotic drilling machine. Clin Oral Implants Res. 2002;13(6):651-656.
- Wat PY, Chow TW, Luk HW, Comfort MB. Precision surgical template for implant placement: a new systematic approach. Clin Implant Dent Relat Res. 2002;4(2):88-92.
- van Steenberghe D, Naert I, Andersson M, Brajnovic I, Van Cleynenbreugel J, Suetens P. A custom template and definitive prosthesis allowing immediate implant loading in the maxilla: a clinical report. Int J Oral Maxillofac Implants. 2002;17(5):663-670.
- Tardieu PB, Vrielinck L, Escolano E. Computer-assisted implant placement. A case report: treatment of the mandible. Int J Oral Maxillofac Implants. 2003;18(4):599-604.
- Vrielinck L, Politis C, Schepers S, Pauwels M, Naert I.Image-based planning and clinical validation of zygoma and pterygoid implant placement in patients with severe bone atrophy using customized drill guides. Preliminary results from a prospective clinical follow-up study. Int J Oral Maxillofac Surg. 2003;32(1):7-14.
- Kopp KC, Koslow AH, Abdo OS. Predictable implant placement with a diagnostic/surgical template and advanced radiographic imaging. J Prosthet Dent. 2003;89(6):611-615.
- Parel SM, Triplett RG. Interactive imaging for implant planning, placement, and prosthesis construction. J Oral Maxillofac Surg. 2004;62(9):41-47.
- Schropp L, Wenzel A, Kostopoulos L. Impact of conventional tomography on prediction of the appropriate implant size. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2001;92(4):458-463.
- Almog DM, Benson BW, Wolfgang L, Frederiksen NL, Brooks SL. CT-Based Imaging and Surgical Guidance in Oral Implantology. J Oral Implantol. 2006;32(1):14-8.