Soft Tissue Calcifications in the Neck:
|
|
Calcifications of the soft tissue structures in the head and neck can occur either as physiological or pathological mineralization. Pathological mineralization is more likely to occur in articular cartilage, vascular tissues, ligaments and glandular tissues and is usually associated with chronic inflammation or scarring. The deposition of mineral salts in dead or degenerating tissues is referred to as dystrophic calcification. In the craniofacial region, these calcifications can occur in the brain (e.g. calcification of choroid plexus, pineal gland, or dura mater), the temporomandibular joint synovial tissue (e.g. synovial chondromatosis), paranasal sinuses (e.g. antrolith), associated with maxilla and mandible (e.g. sialiliths) or in the neck and adjacent structures.
Among patients presenting for dental treatment, some calcifications may be detected on panoramic radiography because of the proximity of soft tissue structures to the focal trough. However, these images are inherently planar and two-dimensional (2D), so localization and therefore diagnosis is problematic. With the increasing use of cone beam computed tomography (CBCT) in dentistry, the incidental discovery of these calcifications is most likely to increase. In addition, CBCT provides images in the third dimension (3D) which facilitates precise localization. The purpose of this article is to describe the imaging characteristics of regional neck calcifications on cone beam computed tomography (CBCT) commonly observed in dental practice. Proper knowledge and diagnosis of these calcifications assists the clinician in the appropriate management of the patient. |
STRATEGIES FOR CBCT INTERPRETATION
Interpretation of CBCT images for calcifications in the neck involves three considerations:
Calcifications of soft tissue structures are a relatively common occurrence. Khan et al.1 recently reviewed 308 CBCT scans (mean age; 52 ± 18 yrs.: age range; 7 - 86 yrs: sex; 56.8% women/43.2% men) and found that 35% had some form of soft tissue calcification with most (90%) in the neck. The most common soft tissue calcifications found, with an almost equal distribution, were carotid artery calcifications (CAC), calcifications of the triticeous cartilage (CTC) or calcifications of the tonsils (CT).
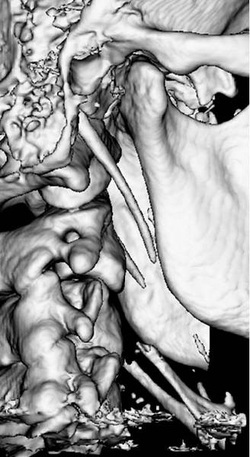
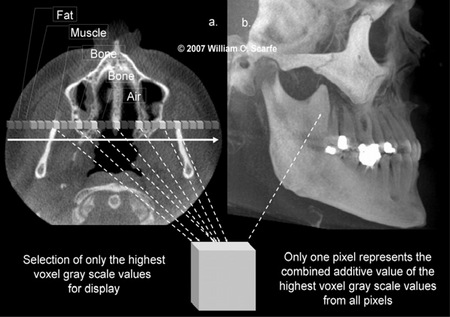
Task specific image display should be used to demonstrate the presence and location of calcifications. Because the key to differential diagnosis is determining the anatomic location of the calcification, an appropriate display mode should be used to provide the optimal viewing. The protocol we recommend uses of medium thickness slice (20mm - 40mm) maximum intensity projection (MIP) images.2 This technique is faster and less expensive than direct volumetric reconstruction (Fig. 1) and, when used in all three orthogonal projections, provides adequate three dimensional information for diagnosis.
Interpretation of CBCT images for calcifications in the neck involves three considerations:
Calcifications of soft tissue structures are a relatively common occurrence. Khan et al.1 recently reviewed 308 CBCT scans (mean age; 52 ± 18 yrs.: age range; 7 - 86 yrs: sex; 56.8% women/43.2% men) and found that 35% had some form of soft tissue calcification with most (90%) in the neck. The most common soft tissue calcifications found, with an almost equal distribution, were carotid artery calcifications (CAC), calcifications of the triticeous cartilage (CTC) or calcifications of the tonsils (CT).
Task specific image display should be used to demonstrate the presence and location of calcifications. Because the key to differential diagnosis is determining the anatomic location of the calcification, an appropriate display mode should be used to provide the optimal viewing. The protocol we recommend uses of medium thickness slice (20mm - 40mm) maximum intensity projection (MIP) images.2 This technique is faster and less expensive than direct volumetric reconstruction (Fig. 1) and, when used in all three orthogonal projections, provides adequate three dimensional information for diagnosis.
Knowledge of the imaging characteristics of the calcification assists in developing a differential diagnosis and facilitates appropriate management. Most calcifications in the maxillofacial region are relatively benign in nature and are associated with few negative outcomes, however in the neck it is necessary to specifically identify carotid artery calcifications (CAC) from others as the presentation of these could lead to more ominous sequelae. Therefore the clinician should have a solid foundation in the radiographic presentation of calcifications condition as it relates to the various structures, particularly on CBCT imaging.
CALCIFICATIONS IN THE NECK
Calcified Stylohyoid Chain (CSC). The styloid process (SP) is a slender projection of bone that arises from the inferior surface of the temporal bone just beneath the external auditory meatus. Within the neck, the SP extends infero-medially towards the pharyngeal wall lateral to the tonsillar fossa. The normal length in an adult is considered to between 20mm3to 30mm4,5 with 40mm considered to be elongated. There are several ligaments (stylohyoid and stylomandibular) and muscles (styloglossus, stylohyoid and stylopharyngeus) that originate from the SP which together act to stabilize the hyoid bone during normal oropharyngeal functions. In particular, the stylohyoid ligament (SHL) arises from the tip of the SP and attaches to the lesser cornu of the hyoid bone. This anatomic arrangement is collectively referred to as the stylohyoid chain. Excessive or abnormal calcification of stylohyoid chain (CSC) components includes elongation of the SP6,7 and calcification of the stylohyoid ligament.8-10 Depending on the population sample, between approximately 1.4%11to 30%6 of individuals have radiographic evidence of CSC, most of which (75%) are bilateral.7 Most patients with CSC are asymptomatic however approximately 1%9 to 10%6 may have clinical symptoms due to the compression of the rigid stylohyoid compressing or irritating nearby structures,12 such as the carotid artery - known as "Eagle's" or "Elongated Styloid Process" Syndrome.
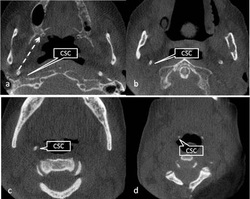
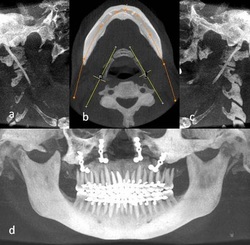
On panoramic radiology, the CSC appears as an elongated slender bony projection that continues from the SP and extends towards, and occasionally appearing continuous with, the lesser cornu of the hyoid bone. Calcification may present in one of 12 patterns13 with variations in degree of ossification, segmentation, pseudo-articulation, thickness and angulation. On axial CBCT images CSC appears as a discrete circular corticated opacification and, because of the caudal, medial and anterior progression presents more anteriorly and medially on progressively more inferior sections (Fig. 2). Our protocol clearly demonstrates the anatomic relationships (Fig. 3).
CALCIFICATIONS IN THE NECK
Calcified Stylohyoid Chain (CSC). The styloid process (SP) is a slender projection of bone that arises from the inferior surface of the temporal bone just beneath the external auditory meatus. Within the neck, the SP extends infero-medially towards the pharyngeal wall lateral to the tonsillar fossa. The normal length in an adult is considered to between 20mm3to 30mm4,5 with 40mm considered to be elongated. There are several ligaments (stylohyoid and stylomandibular) and muscles (styloglossus, stylohyoid and stylopharyngeus) that originate from the SP which together act to stabilize the hyoid bone during normal oropharyngeal functions. In particular, the stylohyoid ligament (SHL) arises from the tip of the SP and attaches to the lesser cornu of the hyoid bone. This anatomic arrangement is collectively referred to as the stylohyoid chain. Excessive or abnormal calcification of stylohyoid chain (CSC) components includes elongation of the SP6,7 and calcification of the stylohyoid ligament.8-10 Depending on the population sample, between approximately 1.4%11to 30%6 of individuals have radiographic evidence of CSC, most of which (75%) are bilateral.7 Most patients with CSC are asymptomatic however approximately 1%9 to 10%6 may have clinical symptoms due to the compression of the rigid stylohyoid compressing or irritating nearby structures,12 such as the carotid artery - known as "Eagle's" or "Elongated Styloid Process" Syndrome.
On panoramic radiology, the CSC appears as an elongated slender bony projection that continues from the SP and extends towards, and occasionally appearing continuous with, the lesser cornu of the hyoid bone. Calcification may present in one of 12 patterns13 with variations in degree of ossification, segmentation, pseudo-articulation, thickness and angulation. On axial CBCT images CSC appears as a discrete circular corticated opacification and, because of the caudal, medial and anterior progression presents more anteriorly and medially on progressively more inferior sections (Fig. 2). Our protocol clearly demonstrates the anatomic relationships (Fig. 3).
Figure 2: Location of CSC on axial images. At the level of the sigmoid notch (a), discrete circular opacities are present posterior and lateral to the pharyngeal airspace, anterior to the petrous temporal bone and posterior and medial to the distal border of the ramus. At the level of the mid ramus/ C1 (b) and mid mandible/C2 (c) the location of the opacity changes along a medial anterior path (arrow in (a)) such that at the level of the lower border of the mandible (d) the opacities are anterior to the airway.
Figure 3: Definitive characterization of the CSC is provided by bilateral oblique linear medium thickness (40mm) MIP images (a/c) developed on axial MIP image at the level of the mandible (b ? yellow line). Panoramic MPR images (d) (orange line on b) are also useful.
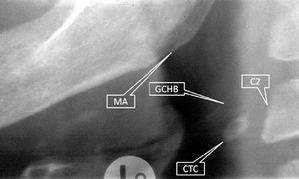
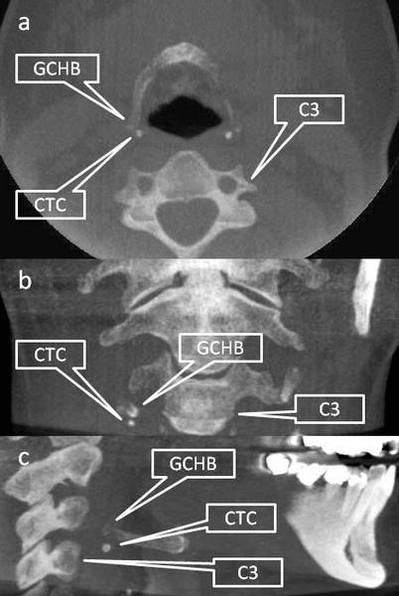
Calcified Triticeous Cartilage (CTC). The triticeous cartilages (TC) are small bilateral ovoid structures located below the hyoid bone in the lateral thyrohyoid ligament at approximately the level of C3-C4. Benign dystrophic calcification of this structure is common, ranging from 5-29%.14 The TC may help reinforce the lateral thyrohyoid ligament.15 When calcified, the TC may be seen on a panoramic radiograph as a single faint opacification immediately inferior to the tip of the greater cornu of the hyoid bone (GCHB) in the same regional area as other dystrophic calcifications of soft tissue including the CAC (Fig 4). On axial CBCT imaging, CTC appears as a single "rice grain" like ovoid homogeneous dense opacification always located medio-posterior to the most distal extent of the GCHB and in the superficial soft tissue in the lateral pre-vertebral space (Fig. 5a). On coronal images CTC are immediately inferior to the GCHB (Fig. 5b) whereas on sagittal images, CTC are immediately inferior and slightly anterior to the GCHB (Fig. 5c).
Calcified Triticeous Cartilage (CTC). The triticeous cartilages (TC) are small bilateral ovoid structures located below the hyoid bone in the lateral thyrohyoid ligament at approximately the level of C3-C4. Benign dystrophic calcification of this structure is common, ranging from 5-29%.14 The TC may help reinforce the lateral thyrohyoid ligament.15 When calcified, the TC may be seen on a panoramic radiograph as a single faint opacification immediately inferior to the tip of the greater cornu of the hyoid bone (GCHB) in the same regional area as other dystrophic calcifications of soft tissue including the CAC (Fig 4). On axial CBCT imaging, CTC appears as a single "rice grain" like ovoid homogeneous dense opacification always located medio-posterior to the most distal extent of the GCHB and in the superficial soft tissue in the lateral pre-vertebral space (Fig. 5a). On coronal images CTC are immediately inferior to the GCHB (Fig. 5b) whereas on sagittal images, CTC are immediately inferior and slightly anterior to the GCHB (Fig. 5c).
Figure 4: Cropped panoramic image of the lower left mandibular angle (MA) demonstrating relationship of the calcified triticeous cartilage (CTC) to the greater cornu of the hyoid bone (GCHB) and second cervical vertebrae (C2).
Figure 5: Axial (a), coronal (b) and sagittal (c) MIP projections showing appearance and location of the CTC immediately inferior to the maximal extension of the greater cornu of the hyoid bone (GCHB).
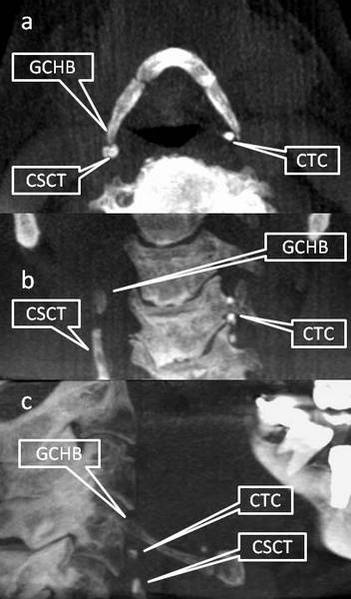
Calcified Superior Cornu of the Thyroid Cartilage (CSCT). The thyroid is the largest and most superior of the cartilages of the larynx and is suspended immediately below the hyoid bone by the thyrohyoid membrane, median and lateral throhyoid ligaments. The latter extends from the terminal portion of the GCHB inferior to a lateral prominence called the superior cornu of the thyroid cartilage. In the thyroid cartilage, calcification is a progressive condition16 that normally starts at the posterior border, the lower margin, and the inferior horn of the thyroid cartilage and is completed around the age of 70 years.17 CSCT on panoramic imaging18 only occurs in older individuals and presents in the same regional location as the CTC and more importantly the CAC.15 On CBCT most often appears as a discontinuous anteroinferiorly perpendicular extension of the terminal end of the greater cornu of the hyoid. On axial sections the CSCT appears as a single distinct circular opacification immediately posterior to the GCHB (Fig. 6a) rather than medial as with the CTC. On coronal sections the CSCT appears as a linear cylindrical opacification extending inferior from the greater cornu of the hyoid (Fig. 6b) and on sagittal images (Fig. 6c) a single peripherally corticated opacification is usually located along a line projected inferiorly and slightly anterior to the most posterior extent of the GCHB.
Calcified Superior Cornu of the Thyroid Cartilage (CSCT). The thyroid is the largest and most superior of the cartilages of the larynx and is suspended immediately below the hyoid bone by the thyrohyoid membrane, median and lateral throhyoid ligaments. The latter extends from the terminal portion of the GCHB inferior to a lateral prominence called the superior cornu of the thyroid cartilage. In the thyroid cartilage, calcification is a progressive condition16 that normally starts at the posterior border, the lower margin, and the inferior horn of the thyroid cartilage and is completed around the age of 70 years.17 CSCT on panoramic imaging18 only occurs in older individuals and presents in the same regional location as the CTC and more importantly the CAC.15 On CBCT most often appears as a discontinuous anteroinferiorly perpendicular extension of the terminal end of the greater cornu of the hyoid. On axial sections the CSCT appears as a single distinct circular opacification immediately posterior to the GCHB (Fig. 6a) rather than medial as with the CTC. On coronal sections the CSCT appears as a linear cylindrical opacification extending inferior from the greater cornu of the hyoid (Fig. 6b) and on sagittal images (Fig. 6c) a single peripherally corticated opacification is usually located along a line projected inferiorly and slightly anterior to the most posterior extent of the GCHB.
Figure 6: Axial (a), coronal (b) and sagittal (c) MIP projections showing appearance and location of the CSCT immediately inferior to the maximal extension of the greater cornu of the hyoid bone (GCHB). CTC can be differentiated from the CSCT on axial images image as being medial to the GCHB (a).
Calcified Tonsils (CT). The tonsils are paired bilateral lymphoid tissue located in the lateral wall of the oropharynx adjacent lateral to the terminal sulcus of the tongue. Tonsilloliths are small areas of calcareous matter that form in the tonsillar crypts which may grow or coalesce to a large size.19 Patients may be asymptomatic or complain of persistent throat irritation, foul taste and odor or otalgia. Tonsilloliths are a common incidental imaging finding on up to 16% of patients.20 On panoramic images they appear as multiple small opaque masses superimposed on the anterior border of the oropharyngeal airway space and may extend over the mandible. On CBCT imaging CT appear as multiple clustered "rice grain" like ovoid homogeneous dense opacifications immediately superficial to the lateral oro-pharyngeal airway space which differentiates them from CAC or CTC (Fig. 7).
Calcified Tonsils (CT). The tonsils are paired bilateral lymphoid tissue located in the lateral wall of the oropharynx adjacent lateral to the terminal sulcus of the tongue. Tonsilloliths are small areas of calcareous matter that form in the tonsillar crypts which may grow or coalesce to a large size.19 Patients may be asymptomatic or complain of persistent throat irritation, foul taste and odor or otalgia. Tonsilloliths are a common incidental imaging finding on up to 16% of patients.20 On panoramic images they appear as multiple small opaque masses superimposed on the anterior border of the oropharyngeal airway space and may extend over the mandible. On CBCT imaging CT appear as multiple clustered "rice grain" like ovoid homogeneous dense opacifications immediately superficial to the lateral oro-pharyngeal airway space which differentiates them from CAC or CTC (Fig. 7).
Figure 7: Orthogonal sections showing CT on axial (a), coronal (b) and sagittal (c) MIP projections as multiple small opacifications superficial and antero-lateral to the oro-pharyngeal airway space. On coronal section (b), clusters are often superimposed over the anterior tubercle of the cervical spine and span supero-inferiorly linearly in line with the pterygoid plates whereas on sagittal sections (c), they are superimposed over the shadow of the oro-pharyngeal airway space or anterior to it.
Carotid Artery Calcifications (CAC). The carotid artery provides the main blood supply to the brain. Atherosclerosis is a pathological condition of the vasculature where vascular plaques form reducing the luminal diameter. This occurs most often at areas of greatest shear force such as the bifurcation of the internal and external carotid artery, located lateral and inferior to the hyoid bone. Atherosclerotic conditions of a carotid artery can lead to neural ischemia (inadequate oxygen to the brain) thus resulting in a cerebrovascular accident (CVA), or stroke. Atheroma-related formations of thrombi and emboli in the carotid artery is the most frequent cause of stroke.21 Calcification is a complication in the evolution of atheromatous plaque enabling potential detection by maxillofacial imaging. Since 198122 calcified atherosclerotic lesions at the carotid bifurcation have been reported on panoramic radiographs as curvilinear irregular parallel radiopacities about 1.5 to 2.5 cm inferiorposterior to the angle of the mandible adjacent to the cervical spine at or below the third and fourth cervical vertebra and inferior and lateral to the hyoid bone.
The prevalence of CAC on panoramic images in the general dental population over 50 years varies from 0.1% to 3.2% increasing with age and is substantially higher (22% to 37%) in populations exhibiting atherosclerotic (hypertension, cardiovascular disease, past stroke/CVA, transient ischaemic attacks or diabetes) or other (hypercholesterolemia, obesity and physical inactivity, cigarette smoking, sleep apnea, head and neck radiation therapy, and male gender) risk factors.
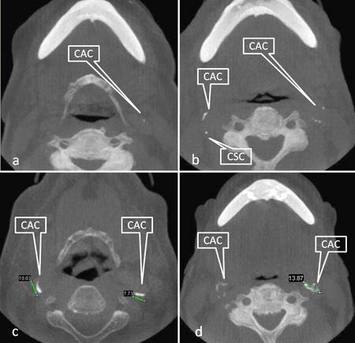
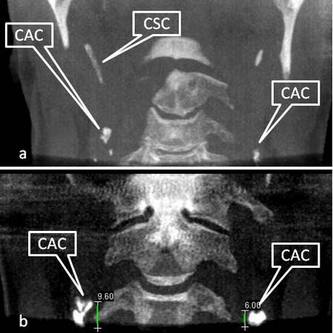
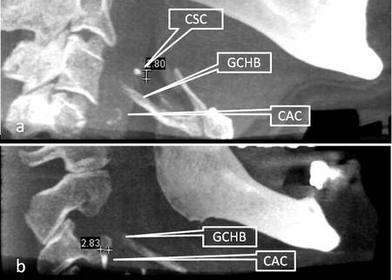
On CBCT imaging, the salient features depend on orthogonal section. On axial projections, most CAC presented as single or multiple "rice grains", linear, or curvilinear homogeneous opacifications (Fig. 8). They are most commonly located in the soft tissue approximately 0-10mm antero-laterally to the anterior tubercle of the transverse process, lateral or more often latero-posterior to the GCHB. They are always postero-lateral to the pharyngeal airway space. In coronal sections, CAC are lateral to the anterior tubercle of the cervical vertebrae (Fig. 9). On sagittal sections, CAC are medial and inferior to the angle of the mandible, lateral and mostly anterior to the cervical tubercle with vertical position varying from C3 to C5 (Fig. 10).
Carotid Artery Calcifications (CAC). The carotid artery provides the main blood supply to the brain. Atherosclerosis is a pathological condition of the vasculature where vascular plaques form reducing the luminal diameter. This occurs most often at areas of greatest shear force such as the bifurcation of the internal and external carotid artery, located lateral and inferior to the hyoid bone. Atherosclerotic conditions of a carotid artery can lead to neural ischemia (inadequate oxygen to the brain) thus resulting in a cerebrovascular accident (CVA), or stroke. Atheroma-related formations of thrombi and emboli in the carotid artery is the most frequent cause of stroke.21 Calcification is a complication in the evolution of atheromatous plaque enabling potential detection by maxillofacial imaging. Since 198122 calcified atherosclerotic lesions at the carotid bifurcation have been reported on panoramic radiographs as curvilinear irregular parallel radiopacities about 1.5 to 2.5 cm inferiorposterior to the angle of the mandible adjacent to the cervical spine at or below the third and fourth cervical vertebra and inferior and lateral to the hyoid bone.
The prevalence of CAC on panoramic images in the general dental population over 50 years varies from 0.1% to 3.2% increasing with age and is substantially higher (22% to 37%) in populations exhibiting atherosclerotic (hypertension, cardiovascular disease, past stroke/CVA, transient ischaemic attacks or diabetes) or other (hypercholesterolemia, obesity and physical inactivity, cigarette smoking, sleep apnea, head and neck radiation therapy, and male gender) risk factors.
On CBCT imaging, the salient features depend on orthogonal section. On axial projections, most CAC presented as single or multiple "rice grains", linear, or curvilinear homogeneous opacifications (Fig. 8). They are most commonly located in the soft tissue approximately 0-10mm antero-laterally to the anterior tubercle of the transverse process, lateral or more often latero-posterior to the GCHB. They are always postero-lateral to the pharyngeal airway space. In coronal sections, CAC are lateral to the anterior tubercle of the cervical vertebrae (Fig. 9). On sagittal sections, CAC are medial and inferior to the angle of the mandible, lateral and mostly anterior to the cervical tubercle with vertical position varying from C3 to C5 (Fig. 10).
Figure 8: Axial projections demonstrating CAC as single rice grain (a), multiple "rice grains" (b - right), linear (b - left; c - right), or curvilinear (c - left; d - left) homogeneous opacifications. As the size of the CAC increases, the number of ipsilateral opacifications also tends to increased (d - left) forming larger coalescing masses (d - right). The proximity to the calcified stylohyoid chain (CSC) is clearly evident.
Figure 9: Coronal MIP projections demonstrating CAC lateral to the cervical vertebrae and presentation as linear globular (a) or globular calcifications (b). Relationship to the calcified stylohyoid chain (CSC) is evident.
Figure 10: Sagittal MIP projections demonstrating location of CAC in relation to the hyoid bone at the level of the greater cornu of the hyoid bone (GCHB). An isolated calcified stylohyoid chain (CSC) is shown.
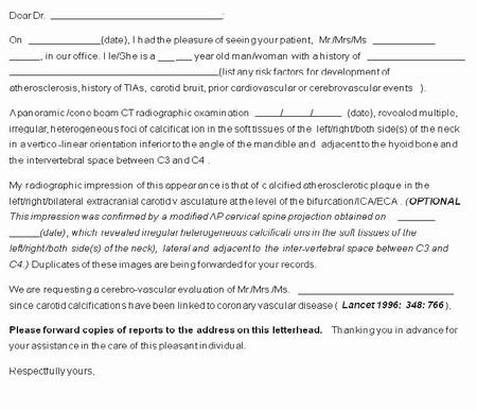
Because of the significant morbidity and mortality of the presence of a CAC, when suspected, the patient should be referred to an appropriate medical physician (Fig. 11) who will confirm the presence and degree of stenosis of the lumen of the artery (usually by duplex ultrasonography) which which is directly related to the risk of a stroke.
Because of the significant morbidity and mortality of the presence of a CAC, when suspected, the patient should be referred to an appropriate medical physician (Fig. 11) who will confirm the presence and degree of stenosis of the lumen of the artery (usually by duplex ultrasonography) which which is directly related to the risk of a stroke.
Figure 11: Example of suggested referral letter to a physician with suspected CAC identified on either a panoramic or CBCT image.
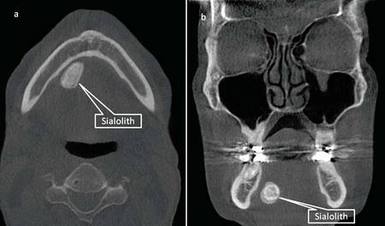
Other Neck Calcifications. Three other calcifications with substantially reduced prevalence may occur in the neck. A sialolith (a.k.a. salivary stone or salivary gland calculus) is an aggregation of calcified material found within the ducts or glandular tissue of salivary glands. The overall on panoramic radiographs in the general population is 0.1%.23 The submandibular gland is the most commonly affected (approx. 80%). Stones in this gland are located near the hilum of the gland or in the proximal portion of Wharton's duct (Fig. 12). Depending on the position of the hyoid bone at the time of the CBCT, a sialolith may appear to be present within the superior neck. They may appear as single linear or globular homogeneous opacities medial to the angle of the mandible.
Other Neck Calcifications. Three other calcifications with substantially reduced prevalence may occur in the neck. A sialolith (a.k.a. salivary stone or salivary gland calculus) is an aggregation of calcified material found within the ducts or glandular tissue of salivary glands. The overall on panoramic radiographs in the general population is 0.1%.23 The submandibular gland is the most commonly affected (approx. 80%). Stones in this gland are located near the hilum of the gland or in the proximal portion of Wharton's duct (Fig. 12). Depending on the position of the hyoid bone at the time of the CBCT, a sialolith may appear to be present within the superior neck. They may appear as single linear or globular homogeneous opacities medial to the angle of the mandible.
Figure 12: Axial (a) and coronal (b) 0.4mm orthogonal sections demonstrating large isolated onion shaped calcification adjacent the lingual cortical plate in the right submandibular region consistent with a sialolith. The patient was asymptomatic and unaware of the condition, however once made aware of the calcification, reported the removal of a similar "stone" on the left time approximately 10 years previously
Lymph nodes are present in the neck in the submandibular, submental preauricular, and cervical areas. Calcification is asymptomatic and usually present in patients who have a history of chronic inflammation in the area (e.g. sinusitis, tonsillitis) however can be the result of tuberculosis, metastases of thyroid cancer or associated with a patients who have been treated for lymphoma. Radiographically these calcifications usually appear as distinct, irregularly shaped opacities characteristically described as "cauliflower-like." As cervical lymph nodes are grouped both superficially and deep to the neck, imaging differentiation is most often based on appearance.
A phlebolith is a calcified vascular thrombus that is most frequently associated with a vein, venule, or hemangioma not contained within bone. Their formation is thought to be as a result of vascular anomaly, which induces thrombus formation. The end result is calcium deposit with eventual stone formation. They are usually multiple, laminated spherical radiopacities with an "onion-like" appearance. The presence of a phlebolith is highly suggestive of either a hard of soft tissue haemangioma
CONCLUSION
Calcifications within the cervical neck at the peri-hyoid region are common findings on CBCT images of this region. An appreciation of the CBCT imaging features of the most frequently (e.g. carotid artery calcifications, calcifications of the triticeous cartilage or calcifications of the tonsils) as well as less commonly occurring conditions is necessary to identify and appropriately refer those with carotid artery calcification for more comprehensive diagnostic medical assessment.
This article was originally submitted to the Australian Dental Journal.
Dr. William C. Scarfe and Dr. Allan Farman hold exclusive rights to this article.
Lymph nodes are present in the neck in the submandibular, submental preauricular, and cervical areas. Calcification is asymptomatic and usually present in patients who have a history of chronic inflammation in the area (e.g. sinusitis, tonsillitis) however can be the result of tuberculosis, metastases of thyroid cancer or associated with a patients who have been treated for lymphoma. Radiographically these calcifications usually appear as distinct, irregularly shaped opacities characteristically described as "cauliflower-like." As cervical lymph nodes are grouped both superficially and deep to the neck, imaging differentiation is most often based on appearance.
A phlebolith is a calcified vascular thrombus that is most frequently associated with a vein, venule, or hemangioma not contained within bone. Their formation is thought to be as a result of vascular anomaly, which induces thrombus formation. The end result is calcium deposit with eventual stone formation. They are usually multiple, laminated spherical radiopacities with an "onion-like" appearance. The presence of a phlebolith is highly suggestive of either a hard of soft tissue haemangioma
CONCLUSION
Calcifications within the cervical neck at the peri-hyoid region are common findings on CBCT images of this region. An appreciation of the CBCT imaging features of the most frequently (e.g. carotid artery calcifications, calcifications of the triticeous cartilage or calcifications of the tonsils) as well as less commonly occurring conditions is necessary to identify and appropriately refer those with carotid artery calcification for more comprehensive diagnostic medical assessment.
This article was originally submitted to the Australian Dental Journal.
Dr. William C. Scarfe and Dr. Allan Farman hold exclusive rights to this article.
REFERENCES
- Khan Z, Wells A, Scarfe W, Farman A. Cone Beam CT isolation of calcifications in the maxillofacial and cervical soft tis sues: A retrospective analysis. Int J Computer Assist Radiol Surg 2008;3(Suppl 1):S221-S222.
- Scarfe WC, Farman AG. Voxel Vision using Maxillofacial CBCT: Clinical Applications of the Maximum Intensity Projection. X-ray Lab and Imaging Currents. (AADRT Newsletter) 2007;Summer:1-25.
- Miller DB. Eagle's syndrome and the Trauma patient. Funct Ortho. 1997;2264:916-925.
- Feldman VB. Eagle's syndrome: a case of symptomatic calcification of the stylohyoid ligaments. J Can Chiropr Assoc. 2003;47:21-27.
- Eagle WW. The symptoms, diagnosis and treatment of the elongated styloid process. Am Surg. 1962;28:1-5.
- Keur JJ, Campbell JP, McCarthy JF, Ralph WJ. The clinical significance of the elongated styloid process. Oral Surg Oral Med Oral Pathol. 1986;61:399-404.
- Ilguy M, Ilguy D, Guler N, Bayirli G. Incidence of the Type and Calcification Patterns in Patients with Elongated Styloid Process. J Int Med Res. 2005;33:96- 102.
- Carmada AJ, Deschamps C, Forest D. Stylohyoid chain ossification: A discussion of etiology. Oral Surg Oral Med Oral Pathol 1989;67:508-14.
- Langlais RP, Miles DA, Van Dis ML. Elongated and mineralized styholyoid ligament complex: A proposed classification and report of a case of Eagle's syndrome. Oral Surg Oral Med Oral Pathol. 1986;61:527-32.
- Ferrario VF, Sigurta D, Daddona A, Dalloca L, Miani A, Tafuro F, et al. Calcification of the stylohyoid ligament: Incidence and morphoquantitave evaluations. Oral Surg Oral Med Oral Pathol. 1990;69:524-9.
- Gossman JR Jr., Tarsitano JJ. The styloid-stylohyoid syndrome. J Oral Surg 1977;35:555-60.
- Winkler S, Sammartino FJ, Monari JH. Stylohyoid Syndrome. Oral Surg Oral Med Oral Pathol 1981;51:215-7.
- MacDonald-Jankowski DS. Calcification of the styloid complex in Londoners and Hong Kong Chinese. Dentomaxillofac Radiol 2001;30:35-39.
- Ahmad M. Madden R, Perez L. Triticeous cartilage: prevalence on panoramic radiographs and diagnostic criteria. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;99:225-30.
- Carter LC. Discrimination between calcified triticeous cartilage and calcified carotid atheroma on panoramic radiography. Oral Surg Oral MPathol Oral Radilo Endod 2000;108-10
- Salman RA, Kinney LA. Calcified thyroid cartilage. Oral Surg Oral Med Oral Pathol 1990;70:806-807.
- Hately W, Evison G, Samuel E. The pattern of ossification in the laryngeal cartilages: a radiological study. Brit J Radiol 1965;38:585-91.
- Monsour PA, Romaniuk K, Hutchings RD. Soft tissue calcifications in the differential diagnosis of opacities superimposed over the mandible by dental panoramic radiography. Aust Dent J 1991;36:94-101.
- de Moura MD, Madureira DF, Noman-Ferreira LC, Abdo EN, de Aguiar EG, Freire AR. Tonsillolith: a report of three clinical cases. Med Oral Patol Oral Cir Bucal 2007;12:E130-3.
- Aspestrand F, Kolbenstvedt A. Calcifications of the palatine tonsillary region: CT demonstration. Radiology. 1987;165:479-480
- Goldstein LB, Adams R, Alberts MJ et al. Primary prevention of ischemic stroke: a guideline from the American Heart Association/American Stroke Association Stroke Council. Stroke. 2006;37:1583-633.
- Friedlander AH, Lande A, Panoramic radiographic identification of carotid arterial plaques. Oral Surg Oral Med Oral Pathol 1981;52:102-4.
- Lee J-S, Kang B-C. Screening panoramic radiographs in a group of patients visiting a Health Promotion Center. Korean J Oral Maxillofac Radiol 2005; 35 : 199-202
- Altug HA, Buyuksoy V, Okcu KM, Dogan N. Hemangiomas of the head and neck with phleboliths: clinical features, diag nostic imaging, and treatment of 3 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e60-4.