TLDs store absorbed radiation in an excited electron state until it is "read". This involves heat activating each TLD and using a photomultiplier tube to read the visible light intensity emitted when the excited electrons return to their normal state. Variations in the emitted light correspond to the amount of detected radiation. The result is the initial raw data radiation dose. This is best accomplished by a dosimetry monitoring service.
The absorbed dose is calculated from the raw data. Dividing the raw data dose for each TLD by the number of x-ray examinations results in the average absorbed dose per TLD for a single examination expressed in microgray (mGy) units. The absorbed dose to a specific anatomical site is the calculated average of all TLD doses for that site. For our model, this was 41 TLDs for the head and neck bone marrow and 24 for the thyroid.
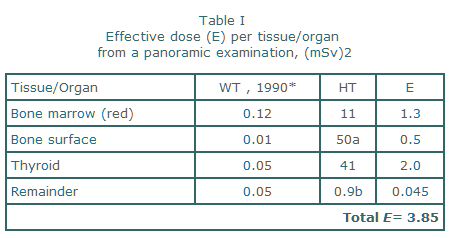
Table I, modified from our reference, exhibits how the data are organized and calculations made using the ICRP recommendations. The critical organs and remainder category for dental radiography are in the first column. Although controversial, any organ not listed was not calculated. The WT, 1990 column is the ICRP numerical radiation sensitivity rating. Higher numbers indicate increased radiation sensitivity. The HT column is the tissue/organ equivalent TLD internal absorbed dose. Bone surface dose and the remainder category, including the brain, required some additional calculations described in the legend under Table I. Column E is calculated by multiplying the numbers for WT, 1990 by those for HT . Total E, expressed in microsievert (mSv), is the sum of all dose effects upon the whole-body. E for the panoramic example is 3.85 mSv.
With E, we can do comparisons for different dental x-ray survey exposures. If E for examination exposure A is 3.85 and for examination B is 7.7, then B produces twice the patient exposure as A. Dividing the E (84 mSv) for a 20 film round collimated full-mouth (FMX) series, as reported by White3, by the panoramic 3.85 shows the FMX to contribute 21.8 times more dose to the patient than the panoramic survey or that 21 panoramic x-rays could be made before exceeding the FMX absorbed dose. Another comparison is to the whole-body background radiation. Annual background dose ranges from 3000 to 4400 mSv3 or 10 to 12 mSv per day. Dividing the FMX 84 mSv by the daily background dose shows the FMX equivalent to 7-10 days of background radiation. In contrast, the panoramic examination 3.85 is approximately 1/3 the daily background. Such accepted life-risk comparisons help patients determine the value of accepting the associated radiation risk for the perceived benefits of the impending radiographic survey.
The absorbed dose is calculated from the raw data. Dividing the raw data dose for each TLD by the number of x-ray examinations results in the average absorbed dose per TLD for a single examination expressed in microgray (mGy) units. The absorbed dose to a specific anatomical site is the calculated average of all TLD doses for that site. For our model, this was 41 TLDs for the head and neck bone marrow and 24 for the thyroid.
Table I, modified from our reference, exhibits how the data are organized and calculations made using the ICRP recommendations. The critical organs and remainder category for dental radiography are in the first column. Although controversial, any organ not listed was not calculated. The WT, 1990 column is the ICRP numerical radiation sensitivity rating. Higher numbers indicate increased radiation sensitivity. The HT column is the tissue/organ equivalent TLD internal absorbed dose. Bone surface dose and the remainder category, including the brain, required some additional calculations described in the legend under Table I. Column E is calculated by multiplying the numbers for WT, 1990 by those for HT . Total E, expressed in microsievert (mSv), is the sum of all dose effects upon the whole-body. E for the panoramic example is 3.85 mSv.
With E, we can do comparisons for different dental x-ray survey exposures. If E for examination exposure A is 3.85 and for examination B is 7.7, then B produces twice the patient exposure as A. Dividing the E (84 mSv) for a 20 film round collimated full-mouth (FMX) series, as reported by White3, by the panoramic 3.85 shows the FMX to contribute 21.8 times more dose to the patient than the panoramic survey or that 21 panoramic x-rays could be made before exceeding the FMX absorbed dose. Another comparison is to the whole-body background radiation. Annual background dose ranges from 3000 to 4400 mSv3 or 10 to 12 mSv per day. Dividing the FMX 84 mSv by the daily background dose shows the FMX equivalent to 7-10 days of background radiation. In contrast, the panoramic examination 3.85 is approximately 1/3 the daily background. Such accepted life-risk comparisons help patients determine the value of accepting the associated radiation risk for the perceived benefits of the impending radiographic survey.
In conclusion, dosimetry is a series of progressive improvements involving methods, assumptions, and interpretation of data. As such, the "magical" number is a current best guessestimate of dose and risk. Despite this, dosimetry data does help us to make evidence-based risk/benefit decisions about how to best use radiation in dentistry and better serve our patients.
REFERENCES
- 1990 Recommendations of the International Commission of Radiological Protection, ICRP Publication 60. Ann ICRP 1990;21:(1-3).
- Danforth, R.A. and Clark, D.E.: Effective dose from radiation absorbed during a panoramic examination with a new generation machine. Oral Surg., Oral Med., Oral Pathol., Oral Radiol Endod 89:236-243, 2000.
- White SC. Assessment of radiation risk from dental radiography. Dentomaxillofac Radiol 1992;21:118-126.