What's wrong with conventional film radiography?
From a Dentomaxillofacial Radiography business viewpoint, disadvantages of analog film are: (1) the cost of consumables including film, and solutions; (2) the investment costs in processing equipment and darkroom space; (3) the manpower and time needed for processing and processor maintainance; (4) time and consumables are needed to mount and label film images; (5) spent processing chemicals being toxic to the environment can be costly to dispose of; and (6) duplicates take time to make and are always inferior to the original. Additional disadvantages of intra-oral film radiography are: (7) that processed film radiographs are rarely optimal in image quality when processed in private dental offices; (8) film is perceived by the patient to be sharp to the tissues; (9) film is easily bent during exposure resulting in a distorted image; and (10) due to low photon efficiency in the absence of a scintillation screen there can be a comparatively high radiation dose. By way of comparison digital imaging: (1) provides time savings when solid-state technology is employed; (2) facilitates communication with the patient when displayed on a computer monitor; (3) eases storage, back-up and retrieval; (4) allows perfect clone duplication of images; (5) permits computed enhancements; (6) eliminates the recurring expenses of film and processing solutions -- and of the disposal of spent solutions; (7) facilitates the use of assessments such as anatomic measurements both for endodontic root length determination and for dental implant planning; (8) opens the way to electronic communication for consultations; and (9) subject to signal-to-noise ratio constraints can allow some reduc-tion in radiation dose. However, as pixel dimensions have declined, the radiation exposure to achieve a suitable signal-to-noise ratio has increased for digital imaging.
What properties are desirable in intra-oral digital x-ray detectors?
Desirable properties for a digital x-ray imaging system include: (1) the image produced is of diagnostic quality; (2) the radiation dose is equal or reduced compared to that necessary to expose analog film; (3) that techniques are compatible with your existing conventional x-ray generators; (4) that the exposure latitude is adequate to reduce the possibility of under- or over-exposure; (5) that the time required for the total procedure should be equal to or less than with film; and (6) that lossless archiving is allowed in an image file format that promotes interoperability within the DICOM standard. Five basic characteristics are: (1) detector active surface area; (2) the ratio of signal-to-noise (SNR); (3) contrast resolution; (4) spatial resolution; and (5) exposure latitude.
From a Dentomaxillofacial Radiography business viewpoint, disadvantages of analog film are: (1) the cost of consumables including film, and solutions; (2) the investment costs in processing equipment and darkroom space; (3) the manpower and time needed for processing and processor maintainance; (4) time and consumables are needed to mount and label film images; (5) spent processing chemicals being toxic to the environment can be costly to dispose of; and (6) duplicates take time to make and are always inferior to the original. Additional disadvantages of intra-oral film radiography are: (7) that processed film radiographs are rarely optimal in image quality when processed in private dental offices; (8) film is perceived by the patient to be sharp to the tissues; (9) film is easily bent during exposure resulting in a distorted image; and (10) due to low photon efficiency in the absence of a scintillation screen there can be a comparatively high radiation dose. By way of comparison digital imaging: (1) provides time savings when solid-state technology is employed; (2) facilitates communication with the patient when displayed on a computer monitor; (3) eases storage, back-up and retrieval; (4) allows perfect clone duplication of images; (5) permits computed enhancements; (6) eliminates the recurring expenses of film and processing solutions -- and of the disposal of spent solutions; (7) facilitates the use of assessments such as anatomic measurements both for endodontic root length determination and for dental implant planning; (8) opens the way to electronic communication for consultations; and (9) subject to signal-to-noise ratio constraints can allow some reduc-tion in radiation dose. However, as pixel dimensions have declined, the radiation exposure to achieve a suitable signal-to-noise ratio has increased for digital imaging.
What properties are desirable in intra-oral digital x-ray detectors?
Desirable properties for a digital x-ray imaging system include: (1) the image produced is of diagnostic quality; (2) the radiation dose is equal or reduced compared to that necessary to expose analog film; (3) that techniques are compatible with your existing conventional x-ray generators; (4) that the exposure latitude is adequate to reduce the possibility of under- or over-exposure; (5) that the time required for the total procedure should be equal to or less than with film; and (6) that lossless archiving is allowed in an image file format that promotes interoperability within the DICOM standard. Five basic characteristics are: (1) detector active surface area; (2) the ratio of signal-to-noise (SNR); (3) contrast resolution; (4) spatial resolution; and (5) exposure latitude.
Detector sensitive area:
Film sizes appropriate for imaging the intra-oral structures were largely achieved by trial and error, but have been remarkably stable for more than 80 years. These are the sizes that are anatomically necessary for the efficient and adequate imaging of the human maxillofacial teeth and their supporting structures. The sensitive x-ray detector areas for digital systems should closely respect the dimensions previously selected for x-ray film, dimensions that have achieved ISO/ ANSI standard recognition. Unfortunately, no such dimension standard exists at this time for digital images used in dentistry. Nevertheless, while the early solid-state intra-oral device surface areas were limited due to the high cost of large CCDs, newer detectors are reaching dimensions that are quite close to those of analog films. Perhaps the marketplace will eventually force detector manufacturers towards the desired detector dimensions, irrespective of guidelines and whether regulations are developed and enforced.
Signal and contrast:
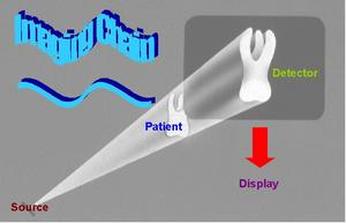
Several stages in the imaging chain are involved in digital radiograph formation. The imaging chain includes the quality of the x-ray beam generated, the differential attenuation of that beam by the patient's tissues, detection of the residual x-rays and their conversion into a radiographic image; display of image and its interpretation. The initiation of the radio-graphic image for solid-state arrays generally is fluoroscopic and captured by a CCD or CMOS chip then converted to a digital signal. For storage phosphors, the analog latent image is emitted following scanning of the exposed photostimulable phosphor plate by a red-emitting solid state laser and digitized following photomultiplication. Given adequate signal and sufficient differences in radiodensities, contrast will be sufficient to differentiate between adjacent structures irrespec-tive of the recording modality and processing used.
Where contrast is not sufficient radiographs might be post-processed to disclose details that would otherwise go undetected. In studies we have conducted at the University of Louisville using perceptibility blocks, all digital detectors tested were equivalent to analog film in being able to detect a defect of .2 mm through 7 mm of aluminum (less than 3% change in density) and several out-performed film in achieving discrimination of .1 mm (e.g. Gendex Visualix HDI; Schick CDR; Trophy RVG-Ultimate).
Spatial Resolution:
Given sufficient tissue radiographic contrast, one could be forgiven for thinking that the ideal images should maximize spatial resolution; however, this is not necessarily the case. It should be remembered that increasing resolution might results in a reduced signal-to-noise ratio unless dose is increased. There is a trade off between dose and resolution that should be viewed as task dependent.
Further, scanning times for photostimulable phosphors are increased if the scanning pitch is narrowed, and the higher the resolution of a digital image the more space it takes to store. It is certainly never warranted to increase the spatial resolution causing time delays with photostimulable phosphor systems or increased dose in the case of solid-state detectors, then to store the image using lossy compression.
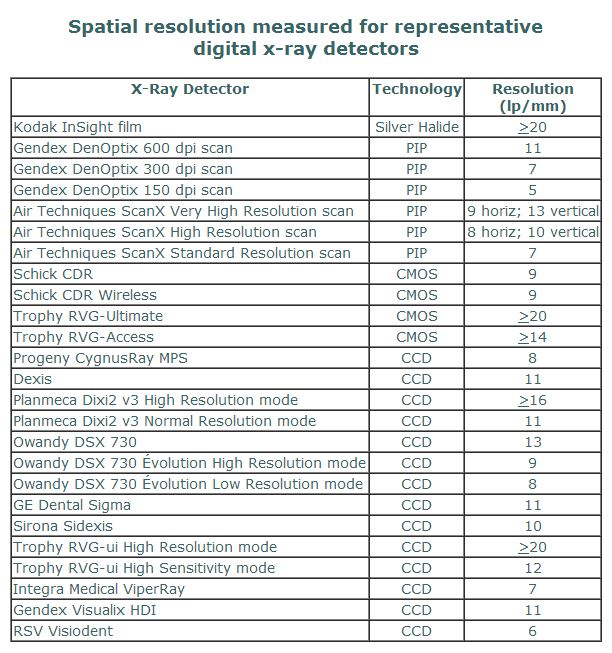
For intra-oral radiography, the detector and the means of developing the latent images represents a series critical components of the imaging chain. Manufacturer claims concerning spatial resolution of digital intra-oral x-ray detectors all too frequently are stipulated to be the "theoretical resolution" based solely upon pixel dimensions of CCD or CMOS chips and not reflecting loss of resolving power due to such factors as light scatter from the scintillator, detector electronics or acquisition software issues. With this in mind, we measured the achieved resolution of a number of digital intra-oral x-ray systems based upon line pair discrimination. Spatial results using a Nuclear Associates line pair phantom are listed below.
Film sizes appropriate for imaging the intra-oral structures were largely achieved by trial and error, but have been remarkably stable for more than 80 years. These are the sizes that are anatomically necessary for the efficient and adequate imaging of the human maxillofacial teeth and their supporting structures. The sensitive x-ray detector areas for digital systems should closely respect the dimensions previously selected for x-ray film, dimensions that have achieved ISO/ ANSI standard recognition. Unfortunately, no such dimension standard exists at this time for digital images used in dentistry. Nevertheless, while the early solid-state intra-oral device surface areas were limited due to the high cost of large CCDs, newer detectors are reaching dimensions that are quite close to those of analog films. Perhaps the marketplace will eventually force detector manufacturers towards the desired detector dimensions, irrespective of guidelines and whether regulations are developed and enforced.
Signal and contrast:
Several stages in the imaging chain are involved in digital radiograph formation. The imaging chain includes the quality of the x-ray beam generated, the differential attenuation of that beam by the patient's tissues, detection of the residual x-rays and their conversion into a radiographic image; display of image and its interpretation. The initiation of the radio-graphic image for solid-state arrays generally is fluoroscopic and captured by a CCD or CMOS chip then converted to a digital signal. For storage phosphors, the analog latent image is emitted following scanning of the exposed photostimulable phosphor plate by a red-emitting solid state laser and digitized following photomultiplication. Given adequate signal and sufficient differences in radiodensities, contrast will be sufficient to differentiate between adjacent structures irrespec-tive of the recording modality and processing used.
Where contrast is not sufficient radiographs might be post-processed to disclose details that would otherwise go undetected. In studies we have conducted at the University of Louisville using perceptibility blocks, all digital detectors tested were equivalent to analog film in being able to detect a defect of .2 mm through 7 mm of aluminum (less than 3% change in density) and several out-performed film in achieving discrimination of .1 mm (e.g. Gendex Visualix HDI; Schick CDR; Trophy RVG-Ultimate).
Spatial Resolution:
Given sufficient tissue radiographic contrast, one could be forgiven for thinking that the ideal images should maximize spatial resolution; however, this is not necessarily the case. It should be remembered that increasing resolution might results in a reduced signal-to-noise ratio unless dose is increased. There is a trade off between dose and resolution that should be viewed as task dependent.
Further, scanning times for photostimulable phosphors are increased if the scanning pitch is narrowed, and the higher the resolution of a digital image the more space it takes to store. It is certainly never warranted to increase the spatial resolution causing time delays with photostimulable phosphor systems or increased dose in the case of solid-state detectors, then to store the image using lossy compression.
For intra-oral radiography, the detector and the means of developing the latent images represents a series critical components of the imaging chain. Manufacturer claims concerning spatial resolution of digital intra-oral x-ray detectors all too frequently are stipulated to be the "theoretical resolution" based solely upon pixel dimensions of CCD or CMOS chips and not reflecting loss of resolving power due to such factors as light scatter from the scintillator, detector electronics or acquisition software issues. With this in mind, we measured the achieved resolution of a number of digital intra-oral x-ray systems based upon line pair discrimination. Spatial results using a Nuclear Associates line pair phantom are listed below.
Acceptable Exposure Range:
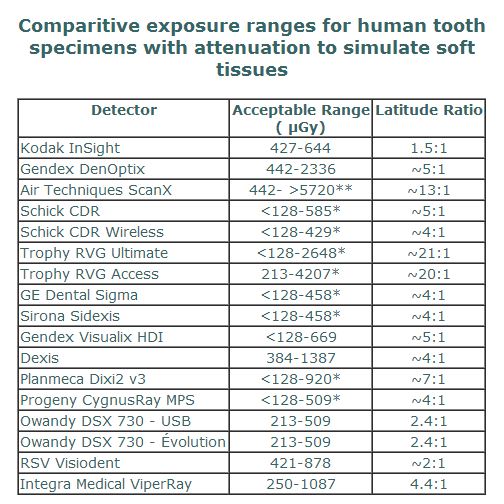
The determination of the acceptable exposure range of a system is task dependent, patient dependent and specimen dependent. To standardize these for comparison between systems for ethical reasons means that a specimen rather than a patient be used. Using mounted extracted teeth and 17 mm acrylic to substitute for soft tissue scatter, it was apparent that the digital systems generally exceeded the acceptable exposure range for F-speed silver halide film. Particularly wide acceptable ranges were found with storage phosphors and with the newly released "SuperCMOS" detectors from Trophy. The positive side of a wide acceptable exposure range is that repeat exposures due to over- or under-exposure are unlikely. The downside is that without judicious use, there is the possibility of using excessive exposure without detriment to the image -- but with increased dosage to the patient.
The determination of the acceptable exposure range of a system is task dependent, patient dependent and specimen dependent. To standardize these for comparison between systems for ethical reasons means that a specimen rather than a patient be used. Using mounted extracted teeth and 17 mm acrylic to substitute for soft tissue scatter, it was apparent that the digital systems generally exceeded the acceptable exposure range for F-speed silver halide film. Particularly wide acceptable ranges were found with storage phosphors and with the newly released "SuperCMOS" detectors from Trophy. The positive side of a wide acceptable exposure range is that repeat exposures due to over- or under-exposure are unlikely. The downside is that without judicious use, there is the possibility of using excessive exposure without detriment to the image -- but with increased dosage to the patient.
Other Considerations:
Any digital system needs to be as efficient and effective as analog film in terms of image quality, safety, ergonomics of practice and economics if it is going to meet with acceptance in the marketplace. We have found solid state detectors to be excellent for operative radiology, for bitewings and selected periapicals to augment a panoramic image and for use with the severely and profoundly mentally retarded for 6-image minipanels. With the latter population, the cable has occasionally been a valuable "fishing line". We have also found the new Schick CDR wireless detector to perform similarly to its wired counterpart in terms of image quality, and the RF transmitter to be able to withstand attempts to jam the signal. One must remember that in going wireless in this way there is the added cost of a disposable battery that costs about $50 per up to 500 exposures.
Any digital system needs to be as efficient and effective as analog film in terms of image quality, safety, ergonomics of practice and economics if it is going to meet with acceptance in the marketplace. We have found solid state detectors to be excellent for operative radiology, for bitewings and selected periapicals to augment a panoramic image and for use with the severely and profoundly mentally retarded for 6-image minipanels. With the latter population, the cable has occasionally been a valuable "fishing line". We have also found the new Schick CDR wireless detector to perform similarly to its wired counterpart in terms of image quality, and the RF transmitter to be able to withstand attempts to jam the signal. One must remember that in going wireless in this way there is the added cost of a disposable battery that costs about $50 per up to 500 exposures.
We have been less happy in the use of photostimulable phosphors for intra-oral radiography than for extraoral radiography. In both cases there is the added scanning time, and need for most systems to unpack the plate in a subdued lighting circumstance, but the real problem is that (unlike extraoral photostimulable phosphor plates) the surface of the intra-oral plate does not have a protective layer. We have found that intra-oral phosphor plates scratch much too readily and need to be discarded and replaced frequently. This can be quite costly over time.
While there are quite a number of bench studies on image quality for various detectors, there is a definite need for more time and motion studies to determine their practicality in everyday use. This would seem to be an area of discovery well suited to the membership of the AADMRT. Furthermore, we need not only to produce prettier images, but also to prove that these images provide a higher standard of care, are not economically prohibitive for the practitioner or society, and that the systems promote efficient and effective workflow within the dental business.
While there are quite a number of bench studies on image quality for various detectors, there is a definite need for more time and motion studies to determine their practicality in everyday use. This would seem to be an area of discovery well suited to the membership of the AADMRT. Furthermore, we need not only to produce prettier images, but also to prove that these images provide a higher standard of care, are not economically prohibitive for the practitioner or society, and that the systems promote efficient and effective workflow within the dental business.