TMJ Imaging: What Should be the Standard of Care?Francisco Eraso, DDS, MS, MS, MSD
Visiting Clinical Associate Professor Indiana University School of Dentistry Department of Oral Facial Development Orthodontics Section From the Winter 2006 AADMRT Newsletter
This brief descriptive paper is not trying to define by any means the standard of TMJ imaging. The goal of this article is to review some concepts for determining what is more appropriate in TMJ diagnosis using imaging as a diagnostic tool.
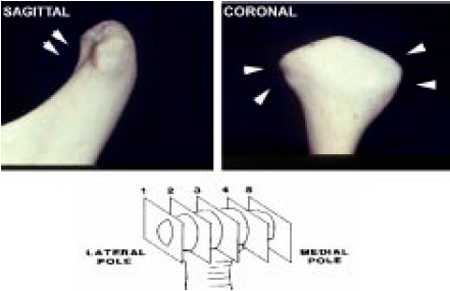
Knowledge of the anatomy of the TMJ is an extremely important component of the diagnostic process, it will help us to determine which imaging technique is the most appropriate in the diagnosis of temporomandibular disorders (TMD). The anatomic components of the TMJ are osseous, soft tissues and other structures (i.e. joint compartments). (Figure 1) |
|
Figure 1: Osseos component of the TMJ complex that can be seen in an image.
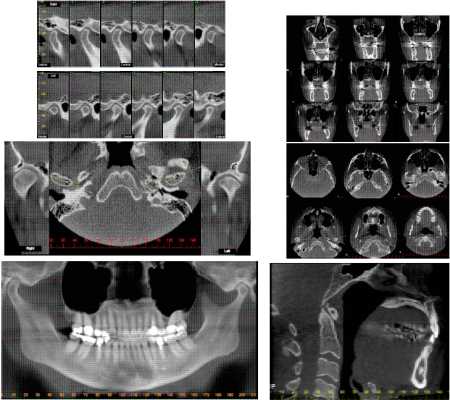
The mandibular condyle is convex along the surface that receives the force, wider in the medio-lateral dimension, and has an oval shape antero-posteriorly. This observation and others, such as the relation of the articular disc with the condyle and the temporal bone, muscle attachments, and occlusion, requires a 3-D approach to analyze the TMJ complex. Sagittal and coronal sections in the imaging of the TMJ are needed to fulfill this requirement. (Figure 2)
The mandibular condyle is convex along the surface that receives the force, wider in the medio-lateral dimension, and has an oval shape antero-posteriorly. This observation and others, such as the relation of the articular disc with the condyle and the temporal bone, muscle attachments, and occlusion, requires a 3-D approach to analyze the TMJ complex. Sagittal and coronal sections in the imaging of the TMJ are needed to fulfill this requirement. (Figure 2)
Figure 2: Sagittal and coronal cuts needed in the 3-D assessment of the TMJ.
In the diagnostic process it is important to differentiate two concepts: differential diagnosis and diagnosis. The first concept refers to the possibilities based on the patient's signs and symptoms while the diagnosis refers to the art of distinguishing one or more entities from others. For this to happen we need to use diagnostic aids, which are instruments or procedures that expedite the diagnostic process (i.e. imaging). These diagnostic aids should be reliable and valid. The diagnostic validity of imaging techniques had been measured in the literature using concepts such as sensitivity (ability to diagnose correctly a condition that actually exists) and specificity (ability to diagnose a condition that actually does NOT exist (false positive) in relation to a "gold standard" (the best instrument, procedure, finding or criteria to recognize a disorder or pathology).
As mentioned before, hard tissues, soft tissues or a combination of both TMJ's structures can be seen in an image. For hard tissue assessment (i.e. bone changes, condylar position) the following common imaging techniques can be considered:
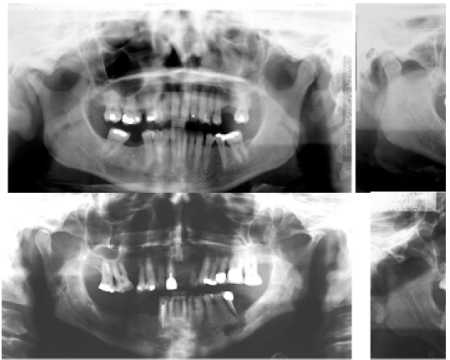
When studies used panoramic imaging (Figure 3) for the same diagnostic task using the same "gold standard", results were as good or better than the transcranial images (sensitivity 81% - specificity 100%).1
But, a question for these studies should be: is tomography the "gold standard"?
In the diagnostic process it is important to differentiate two concepts: differential diagnosis and diagnosis. The first concept refers to the possibilities based on the patient's signs and symptoms while the diagnosis refers to the art of distinguishing one or more entities from others. For this to happen we need to use diagnostic aids, which are instruments or procedures that expedite the diagnostic process (i.e. imaging). These diagnostic aids should be reliable and valid. The diagnostic validity of imaging techniques had been measured in the literature using concepts such as sensitivity (ability to diagnose correctly a condition that actually exists) and specificity (ability to diagnose a condition that actually does NOT exist (false positive) in relation to a "gold standard" (the best instrument, procedure, finding or criteria to recognize a disorder or pathology).
As mentioned before, hard tissues, soft tissues or a combination of both TMJ's structures can be seen in an image. For hard tissue assessment (i.e. bone changes, condylar position) the following common imaging techniques can be considered:
- Transcranials
- Panoramics
- Extraorals (lateral, posterior-anterior, SMV views, etc)
- Tomography
- Computed tomography/Cone Beam Computed Tomography (CT - CBCT).
When studies used panoramic imaging (Figure 3) for the same diagnostic task using the same "gold standard", results were as good or better than the transcranial images (sensitivity 81% - specificity 100%).1
But, a question for these studies should be: is tomography the "gold standard"?
Figure 3: Bone changes of the condyle found in panoramic images.
Submental-vertical (SMV) views help us to minimize technical errors aligning the X-ray beam relative to the condylar axis in the horizontal plane. Ideally, it must be used in combination with other images (tomography) for optimal diagnostic results.
Tomography on the other hand has been considered as one of the best diagnostic aids for the evaluation of the articular spaces, it is optimal in the detection of bone lesions, especially when frontal and sagittal views are taken in combination. Studies using this technique for the detection of osseous defects showed inferior results compared to previous studies (sensitivity 61% - specificity 73%), however, using direct visual exams of autopsy specimens as a "gold standard".2
Computed tomography (CT) is an excellent diagnostic tool that overcomes most of the problems with the techniques previously described: it offers excellent resolution and is effective for the diagnosis of tumors. Even though it is a tool that easily allows 3-D assessment of the TMJ complex, it is not useful for the visualization of soft tissue and requires high levels of radiation. Also, high cost and limited availability are some of its main disadvantages. When reports in the literature used CT for the detection of osseous defects employing tomography as the "gold standard", results were excellent (sensitivity 100% - specificity 94%).3 When direct visual exams of autopsy specimens were used as a "gold standard" results were also very good (sensitivity 75% - specificity 94%).4
Cone beam computed tomography (CBCT) differs from CT in the type of source detector complex and in the method of data acquisition. Because CBCT presently uses one rotation around the patient similar to the panoramic radiography, a complete dento-maxillofacial volume or limited area of interest (i.e. TMJ) can be obtained.5 As far as radiation dose, CBCT is much lower when compared to CT and comparable to a series of dental radiographs when we balanced diagnostic potential, risks and cost. (Table 1)6
Submental-vertical (SMV) views help us to minimize technical errors aligning the X-ray beam relative to the condylar axis in the horizontal plane. Ideally, it must be used in combination with other images (tomography) for optimal diagnostic results.
Tomography on the other hand has been considered as one of the best diagnostic aids for the evaluation of the articular spaces, it is optimal in the detection of bone lesions, especially when frontal and sagittal views are taken in combination. Studies using this technique for the detection of osseous defects showed inferior results compared to previous studies (sensitivity 61% - specificity 73%), however, using direct visual exams of autopsy specimens as a "gold standard".2
Computed tomography (CT) is an excellent diagnostic tool that overcomes most of the problems with the techniques previously described: it offers excellent resolution and is effective for the diagnosis of tumors. Even though it is a tool that easily allows 3-D assessment of the TMJ complex, it is not useful for the visualization of soft tissue and requires high levels of radiation. Also, high cost and limited availability are some of its main disadvantages. When reports in the literature used CT for the detection of osseous defects employing tomography as the "gold standard", results were excellent (sensitivity 100% - specificity 94%).3 When direct visual exams of autopsy specimens were used as a "gold standard" results were also very good (sensitivity 75% - specificity 94%).4
Cone beam computed tomography (CBCT) differs from CT in the type of source detector complex and in the method of data acquisition. Because CBCT presently uses one rotation around the patient similar to the panoramic radiography, a complete dento-maxillofacial volume or limited area of interest (i.e. TMJ) can be obtained.5 As far as radiation dose, CBCT is much lower when compared to CT and comparable to a series of dental radiographs when we balanced diagnostic potential, risks and cost. (Table 1)6
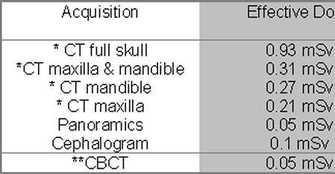
Table 1: Effective dose for different acquisition modes
Multi slice scanner (* Siemens Sensation 64, 120 kV, effective tube current 80mAs, slice thickness 0.75mm & ** Newtom QR DVT 9000, 110 kV, tube current 2.5 mA)
Taking into account all of the advantages of the CBCT to image the TMJ complex, CBCT provides the opportunity to evaluate several areas of interest (i.e. sinuses, airways, etc.). This 3-D approach is a powerful tool for diagnosis, planning, monitoring and evaluation of TMD. (Figure 4) For soft tissue assessment (i.e. disc position) the following most common imaging techniques can be considered:
Multi slice scanner (* Siemens Sensation 64, 120 kV, effective tube current 80mAs, slice thickness 0.75mm & ** Newtom QR DVT 9000, 110 kV, tube current 2.5 mA)
Taking into account all of the advantages of the CBCT to image the TMJ complex, CBCT provides the opportunity to evaluate several areas of interest (i.e. sinuses, airways, etc.). This 3-D approach is a powerful tool for diagnosis, planning, monitoring and evaluation of TMD. (Figure 4) For soft tissue assessment (i.e. disc position) the following most common imaging techniques can be considered:
- Arthrography
- Magnetic resonance imaging (MRI)
Figure 4: CBCT TMJ study
(Courtesy: Dr. David Hatcher . DDI Imaging Center, Roseville, CA).
Arthrography was a technique described in the past to demonstrate its potential value in the diag?nosis of soft tissue derangement of the joint. How?ever, it had few advocates, and the technique it?self for the TMJ had only limited clinical use. The reasons for the skeptical attitude toward this method is attributed to at least 3 disadvantages: 1) difficulty of injecting into the joint compartment, 2) pain for the patient, 3) information gained at the early stage of its development was usually of limited value for treatment planning and evaluation of prognosis.7
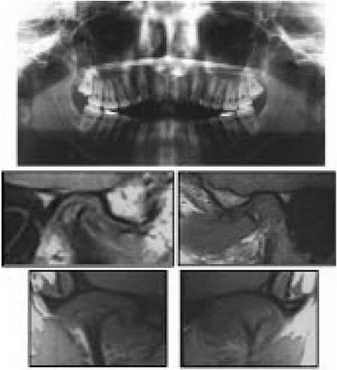
MRI does not use ionizing radiation, making this technique possible to distinguish between soft and hard tissue. It provides excellent images of disc displacement (DD) in multiple planes. However, problems such as cost, availability and claustrophobia need to be taken into consideration. It is important to recognize that MRI results should not dictate the treatment; clinical signs and examinations are more important. MRI is not a routine procedure for most patients. It is indicated when something other than disc displacement (i.e. tumors), prior to intracapsular surgery or when conservative treatment options are not effective. The validity of MRI images for the detection of DD (sagittal & frontal views) using direct visual exams of autopsy specimens as a "gold standard" showed very promising results (sensitivity 86% & 87% - specificity 63% & 80% respectively).8,9(Figure 5)
(Courtesy: Dr. David Hatcher . DDI Imaging Center, Roseville, CA).
Arthrography was a technique described in the past to demonstrate its potential value in the diag?nosis of soft tissue derangement of the joint. How?ever, it had few advocates, and the technique it?self for the TMJ had only limited clinical use. The reasons for the skeptical attitude toward this method is attributed to at least 3 disadvantages: 1) difficulty of injecting into the joint compartment, 2) pain for the patient, 3) information gained at the early stage of its development was usually of limited value for treatment planning and evaluation of prognosis.7
MRI does not use ionizing radiation, making this technique possible to distinguish between soft and hard tissue. It provides excellent images of disc displacement (DD) in multiple planes. However, problems such as cost, availability and claustrophobia need to be taken into consideration. It is important to recognize that MRI results should not dictate the treatment; clinical signs and examinations are more important. MRI is not a routine procedure for most patients. It is indicated when something other than disc displacement (i.e. tumors), prior to intracapsular surgery or when conservative treatment options are not effective. The validity of MRI images for the detection of DD (sagittal & frontal views) using direct visual exams of autopsy specimens as a "gold standard" showed very promising results (sensitivity 86% & 87% - specificity 63% & 80% respectively).8,9(Figure 5)
Figure 5: MRI evaluation (sagittal & frontal views) for an orthodontic patient screened using a panoramic radiograph.
SUMMARY:
A complete assessment of the TMJ requires the knowledge of its components. Panoramic radiographs had been demonstrated to be an excellent screening tool. If tomography is being used to evaluate the osseous components of the TMJ, SMV views should be taken to correct the X-ray beam in relation to the condylar axis at the horizontal plane.
It is clear that 3-D imaging has becoming an essential tool in dentistry. The development of spiral CT, CBCT and MRI has revolutionized the way that we evaluate the TMJ complex. Three dimensional analysis is a powerful tool for planning, monitoring and evaluating the TMJ; however, the accuracy and reliability depends on the correct application of the images obtained. CT images are documented in the literature to be the image of choice for hard tissue assessment,4 however, radiation dose, cost and availability are a concern. CBCT is an excellent choice for a complete 3-D TMJ assessment; however, further studies are needed to confirm its diagnostic validity. MRI definitely is the standard of care for soft tissue assessment; however, it is important to recognize that MRI results should not dictate the treatment. Clinical signs and examinations are not replaced by MRI.
Finally, the ability to interpret the information obtained is proportional to familiarity with the structures and imaging technique. The proper interpretation of images by an oral and maxillofacial radiologist is as important as the images themselves. This approach will enhance treatment planning and its proper clinical application.
SUMMARY:
A complete assessment of the TMJ requires the knowledge of its components. Panoramic radiographs had been demonstrated to be an excellent screening tool. If tomography is being used to evaluate the osseous components of the TMJ, SMV views should be taken to correct the X-ray beam in relation to the condylar axis at the horizontal plane.
It is clear that 3-D imaging has becoming an essential tool in dentistry. The development of spiral CT, CBCT and MRI has revolutionized the way that we evaluate the TMJ complex. Three dimensional analysis is a powerful tool for planning, monitoring and evaluating the TMJ; however, the accuracy and reliability depends on the correct application of the images obtained. CT images are documented in the literature to be the image of choice for hard tissue assessment,4 however, radiation dose, cost and availability are a concern. CBCT is an excellent choice for a complete 3-D TMJ assessment; however, further studies are needed to confirm its diagnostic validity. MRI definitely is the standard of care for soft tissue assessment; however, it is important to recognize that MRI results should not dictate the treatment. Clinical signs and examinations are not replaced by MRI.
Finally, the ability to interpret the information obtained is proportional to familiarity with the structures and imaging technique. The proper interpretation of images by an oral and maxillofacial radiologist is as important as the images themselves. This approach will enhance treatment planning and its proper clinical application.
REFERENCES
- Larheim TA, Johannessen S, Tveito L. Abnormalities of the temporomandibular joint in adults with rheumatic disease. A comparison of panoramic, transcranial and transpharyngeal radiography with tomography. Dentomaxillofac Radiol 1988;17:109-113.
- Rohlin M, Akerman S, Kopp S. Tomography as an aid to detect macroscopic changes of the temporomandibular joint. An autopsy study of the aged. Acta Odontol Scand 1986;44:131-140.
- Manzione JV, Katzberg RW, Brodsky GL, Seltzer SE, Mellins HZ. Internal derangements of the temporomandibular joint: diagnosis by direct sagittal computed tomography. Radiology 1984;150:111-115.
- Westesson PL, Katzberg RW, Tallents RH, Sanchez-Woodworth RE, Svensson SA. CT and MR of the temporomandibular joint: comparison with autopsy specimens. AJR Am J Roentgenol 1987;148:1165-1171.
- Graber TM, Vanarsdall RL, Vig WL. Orthodontics. Current Principles and Techniques. 4th ed.: Elsevier Mosby, 2005:77.
- Swennen GRJ, Schutyser F, Hausamen JE. Three - Dimensional Cephalometry: Springer, 2006:6.
- Katzberg R, Westesson, PL. Diagnosis of the Tempomandibular Joint. 1st ed.: Saunders, 1994:101.
- Tasaki MM, Westesson PL. Temporomandibular joint: diagnostic accuracy with sagittal and coronal MR imaging. Radiology 1993;186:723-729.
- Katzberg RW, Westesson PL, Tallents RH, et al. Temporomandibular joint: MR assessment of rotational and sideways disk displacements. Radiology 1988;169:741-748.