The role of 3D volumetric modeling in
|
|
Essential to surgical treatment is knowledge of the anatomical relationships between vital structures in order to better ensure a favorable treatment outcome. For most of history, determining these relationships has relied upon the knowledge and experienced surgical skills of the operators to offset the lack of transparency of the human body and any unforeseen surgical difficulties encountered had to be managed in real time. However, with the discovery of x-rays and the subsequent developments of conventional tomographic imaging, computed tomography (CT) and magnetic resonance imaging (MRI) the human body became transparent and interpretation and treatment planning entered into the third dimension. For dentistry, the 3D era began in the1980s with the use of medical CT for dental implant treatment planning. This eventually resulted in the development of cone beam computed tomography (CBCT) for dental imaging.
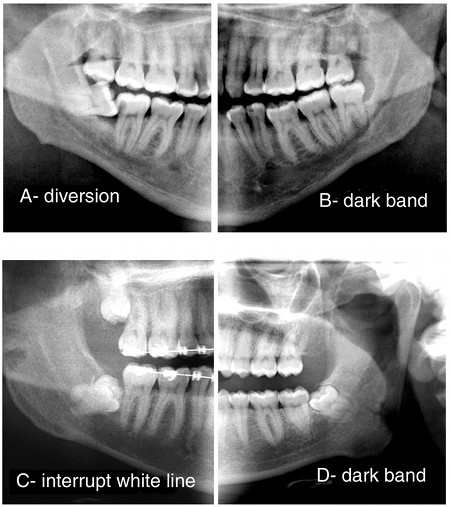
In this decade, the worldwide use of CBCT has dramatically increased amongst all dentists and expanded into other areas of dental treatment beside dental implant and orthodontic imaging. As such, the benefits of CBCT imaging for impacted third molar extractions and localization of the inferior alveolar nerve canal are being realized. The remainder of this article will focus upon the factors associated with interpreting radiographs for mandibular third molar surgery and the role of CBCT as a method of improving interpretation and resultant treatment outcomes. For decades, dental surgeons have made impacted third molar treatment decisions from periapical and primarily panoramic radiographs. To determine what radiographic indicators influenced treatment decisions, Rood et al1 conducted a prospective and retrospective radiographic surveys of 1560 mandibular third molars that either required surgical treatment or had been removed. Using the previously documented seven radiographic signs of increased risk for nerve injury during third molar surgery, the study found that the three signs considered most important as predictors of nerve injury were; diversion of the canal pathway, a darken shadow superimposed upon the roots, and interruption of the white line cortical border of the mandibular canal (See Figs. 1 A-D). Results from this study indicate that impaired labial sensation will be experienced by one in three patients with radiographs showing diversion of the canal and one in four with either darkening of the roots or interruption of the white line cortical border. As such, these findings become a radiographic interpretative guide for risk assessment and prognostication of treatment outcomes. |
However, mere identification of the risk, particularly from a 2D image, doesn't always ensure a favorable treatment outcome. Application of surgical technique also plays a critical role. For imaging to effectively assist technique prior to surgery, it must provide viewing in 3 dimensions. Medical CT provides such imaging analysis and exploring such use of CT for inferior alveolar and lingual nerve assessment was reported in mid 1990s well before the development of CBCT 2. In this regard, Öhman et al3 conducted a study of third molar surgical cases which emphasized the effectiveness of using CT imaging for complicated cases as determined by radiology criteria; particularly seeing a dark band over the molar on plain radiographs. Their review of hospital records of third molar cases from 1996-2000 indicated 5 cases of persistent dysaesthesia occurred. In 2001, after introducing CT imaging to assist treatment planning for complicated cases, no cases of persistent dysaesthesia had developed to the time of their published report in 2006. Such findings advocate using 3D CT imaging for selected complicated cases.
The development of CBCT and the increasing accessibility to 3D imaging for dental purposes makes such imaging analysis a viable treatment planning options when complicated third molar extractions are encountered. Such a study has been recently reported (2008) in which CBCT imaging was found to improve localization of the third molar for presurgical planning4. However, following a medical CT approach to image interpretation may not be the most effective display of complex anatomical relationships for treatment planning purposes especially if a cost effective method could be developed that could improve visualization of these relationships.
For me (RAD), such a concern for improved visualization occurred during the development of a CBCT third molar article with Peck and Hall for the California Dental Journal in 20035. Laboriously viewing numerous images and then attempting to describe with accuracy the interpretation was time consuming and still did not represent a clearly defined picture of the anatomical relationship between the nerve canal and the molar roots. This experience led me to seek other options in the field of visual reconstructed virtual modeling using CBCT data. Such was accomplished at the University of Southern California School of Dentistry Virtual Craniofacial Imaging Laboratory. A digital segmentation process of selected data volume resulted in an interactive virtual model of the molar and mandibular canal which could be separated from the remaining data volume for discreet analyses without other anatomical distractions 6. The resultant models were first presented to the American Academy of Oral and Maxillofacial Radiology during the annual meeting in 2004. The initial reaction was that of impressed by the technology but it was not seen as a practical aid for actual surgical treatment planning due to data construction time and perceived added patient cost to the surgical procedure.
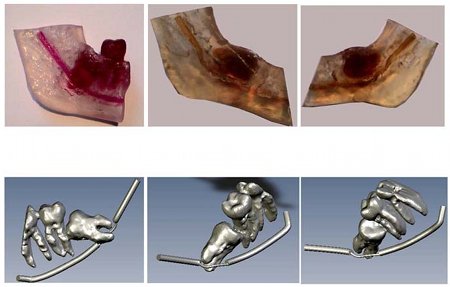
The pursuit of visual modeling to aid treatment planning continued with the development of CBCT generated stereolithography acrylic models (BMI - Biomedical Modeling, Inc. Boston, MA, USA) of the third molar and nerve canal (Fig. 2 A). Such physical models of complex third surgery cases were generated to assist advanced senior dentals at the University of Nevada Las Vegas, School of Dental Medicine (2007) with treatment planning these cases. Although such models were considered extremely helpful by the students for a limited number of six cases, the layering process of making the resin model created seams which hindered clear definition of the internal structures and made it difficult to visualize anything other than a gross assessment.
The development of CBCT and the increasing accessibility to 3D imaging for dental purposes makes such imaging analysis a viable treatment planning options when complicated third molar extractions are encountered. Such a study has been recently reported (2008) in which CBCT imaging was found to improve localization of the third molar for presurgical planning4. However, following a medical CT approach to image interpretation may not be the most effective display of complex anatomical relationships for treatment planning purposes especially if a cost effective method could be developed that could improve visualization of these relationships.
For me (RAD), such a concern for improved visualization occurred during the development of a CBCT third molar article with Peck and Hall for the California Dental Journal in 20035. Laboriously viewing numerous images and then attempting to describe with accuracy the interpretation was time consuming and still did not represent a clearly defined picture of the anatomical relationship between the nerve canal and the molar roots. This experience led me to seek other options in the field of visual reconstructed virtual modeling using CBCT data. Such was accomplished at the University of Southern California School of Dentistry Virtual Craniofacial Imaging Laboratory. A digital segmentation process of selected data volume resulted in an interactive virtual model of the molar and mandibular canal which could be separated from the remaining data volume for discreet analyses without other anatomical distractions 6. The resultant models were first presented to the American Academy of Oral and Maxillofacial Radiology during the annual meeting in 2004. The initial reaction was that of impressed by the technology but it was not seen as a practical aid for actual surgical treatment planning due to data construction time and perceived added patient cost to the surgical procedure.
The pursuit of visual modeling to aid treatment planning continued with the development of CBCT generated stereolithography acrylic models (BMI - Biomedical Modeling, Inc. Boston, MA, USA) of the third molar and nerve canal (Fig. 2 A). Such physical models of complex third surgery cases were generated to assist advanced senior dentals at the University of Nevada Las Vegas, School of Dental Medicine (2007) with treatment planning these cases. Although such models were considered extremely helpful by the students for a limited number of six cases, the layering process of making the resin model created seams which hindered clear definition of the internal structures and made it difficult to visualize anything other than a gross assessment.
This development rekindled the initial interest in the interactive visual segmentation model. Such a basic model (Fig. 2 B) of the molar and mandibular canal was developed (BMI - Biomedical Modeling, Inc, Boston, MA, USA), but student evaluation did not occur due to changes in the surgical faculty overseeing the project. Concerns for use of CBCT and model imaging again focused upon additional patient expense, time to develop the model and possible delayed delivery of care, interpretation time of the clinician, and radiation dose to the patient. However, when we considered the interpretive options within the CBCT image volume to other and probably ineffective imaging modalities the radiation dose was considered low risk to the perceived patient benefit; an opinion shared by others 4.
Recently, an interactive visual model has been developed by Anatomage Inc., San Jose, CA, which address these concerns. Using any CBCT scan data, a fully segmented model of the patient's complete or impacted dentition, inferior alveolar nerve and skeletal anatomy is easily obtainable by clinicians and imaging centers.
Through the AnatoModel service, the CBCT scan is first uploaded online to Anatomage where it can instantly be processed. Once received, the dentition and jaws are segmented out and separated away from the remaining anatomy (Figs 3.). Then each tooth is modeled with an isosurface to show the surface morphology as an opaque 3D visualization. The inferior alveolar nerve, as well as the incisive canal, can also be traced as a bright red model to highlight its orientation in relation to the hard tissues of the teeth and jaws7and 8. For mandibular third molar extractions, this shows precisely where the tooth is located within the bone and the relationship to the inferior alveolar nerve. For impactions such as mesiodens, tracing the incisive canal can also be very valuable.
Recently, an interactive visual model has been developed by Anatomage Inc., San Jose, CA, which address these concerns. Using any CBCT scan data, a fully segmented model of the patient's complete or impacted dentition, inferior alveolar nerve and skeletal anatomy is easily obtainable by clinicians and imaging centers.
Through the AnatoModel service, the CBCT scan is first uploaded online to Anatomage where it can instantly be processed. Once received, the dentition and jaws are segmented out and separated away from the remaining anatomy (Figs 3.). Then each tooth is modeled with an isosurface to show the surface morphology as an opaque 3D visualization. The inferior alveolar nerve, as well as the incisive canal, can also be traced as a bright red model to highlight its orientation in relation to the hard tissues of the teeth and jaws7and 8. For mandibular third molar extractions, this shows precisely where the tooth is located within the bone and the relationship to the inferior alveolar nerve. For impactions such as mesiodens, tracing the incisive canal can also be very valuable.
The data are saved and posted back online in the doctor's and/or imaging center's secure account and made available to download for quick and easily visualization with 3D viewing software. This service eliminates any clinician time involved with the process of segmentation and modeling the anatomy, thus allowing a better focus upon direct delivery of patient care. The effective cost of the service is not expected to add considerable monetary expense to the patient, an imaging center or a referring doctor.
With each tooth and jaw bone individually separated, the processing and software technology also allows for next generation Dynamic CBCT applications, where virtual surgical simulations can be created for treatment planning and patient presentations purposes 8.
This article has provided a brief overview of the role of CT and CBCT in impacted third molar surgery when the inferior alveolar nerve has been identified at risk for injury during surgery. It is suggested that visual reconstructed modeling can enhance visualization of critical anatomical relationships and potentially improve surgical outcomes. A newly developed imaging module is presented which can provide such modeling in a cost effective and timely manner. Evaluation of this imaging technology upon treatment outcomes is in progress.
With each tooth and jaw bone individually separated, the processing and software technology also allows for next generation Dynamic CBCT applications, where virtual surgical simulations can be created for treatment planning and patient presentations purposes 8.
This article has provided a brief overview of the role of CT and CBCT in impacted third molar surgery when the inferior alveolar nerve has been identified at risk for injury during surgery. It is suggested that visual reconstructed modeling can enhance visualization of critical anatomical relationships and potentially improve surgical outcomes. A newly developed imaging module is presented which can provide such modeling in a cost effective and timely manner. Evaluation of this imaging technology upon treatment outcomes is in progress.
REFERENCES
- Rood JP, Shehab BA. The radiological predictor of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 1990; 28:20-25.
- Feifel H, Riediger D, Gustorf-Aeckerle R. High resolution computed tomography of the inferior and lingual nerves.Neuroradiology 1994; 36: 236-238.
- Öhman A, Kivijärvi K, Blombäck U, Flygare L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofacial Radiology 2006; 35: 30-35.
- Neugebauer J, Shirani R, Mischlowski RA, Ritter L et al. Comparison of cone-beam volumetric imaging and combined plain radiographs for localization of the mandibular canal before removal of impacted third molars. Oral Surg Oral Med Oral Path Oral Radiol Endod 2008; 105: 633-642.
- Danforth RA, Peck J, Hall P. Cone beam volume tomography: An imaging option for diagnosis of complex mandibular third molar anatomical relationships. J Calif. Dent Assoc. 2003; 31:847-852.
- Reyes E, Danforth RA, Alexandroni ES, Memon A Mah J. Third molar evaluation with cone-beam computerized tomography. International Journal of Computed Assisted Radiology and Surgery. 2006; 1(2):133-116.
- Mah J, and Redmond R. The evolution of digital study models. Journal of Clinical Orthodontics. September 2007. Volume XLI Number(9) 561.
- Chenin D, Chenin David, Chenin S, Choi J. Dynamic Cone-Beam Computed Tomography in Orthodontic Treatment.Journal of Clinical Orthodontics. August 2009. Volume XLIII Number (8).