NCRP 145 Radiation Protection in Dentistry -
|
|
NCRP Report No. 145 states its guiding principle is to minimize exposure to patients, staff and public through the application of the principle of ALARA3. The report interprets the principle of ALARA as extending to "...further reduction of doses that are already below regulatory limits..." [Emphasis mine] and "...may be extended to patients for whom no regulatory limits exist." The dose limits do not apply to diagnostic or therapeutic exposure of the patient in the healing arts. The report encourages: "...all reasonable efforts should be made to reduce or eliminate avoidable radiation exposure..." Report No. 145 does not become involved in discussing what "reasonable efforts to reduce or eliminate avoidable radiation exposure" might involve, but clearly the intent of the report's 109 recommendations is to eliminate all avoidable radiation exposure, no matter how small or trivial.
In standard NCRP terminology, "shall and shall not" statements indicate adherence to the recommendation is necessary to meet accepted standards of protection; "should and should not" statements are used to indicate prudent practice. In classic understated fashion the report "makes a number of recommendations for the dentist" to achieve the reports defined ALARA goals. NCRP No. 145 then proceeds to make 64 "shall" recommendations, 24 "shall not" recommendations, 15 "should" and 6 "should not" recommendations [total 109], making this a highly prescriptive document, whose intent is almost guaranteed to radically change the way dental radiography is practiced on a daily basis. In contrast, the previous NCRP Report No. 35 only included 30 shall statements, 6 shall not statements and 22 should statements [total 58]
NCRP No. 145 clearly establishes the guidelines for "best practices" in dental radiography, as well as the ultimate extension of the ALARA concept to every facet of dental radiography. The report's recommendations will require dentistry and dental x-ray laboratories to evaluate how dental radiography is currently practiced and at the same time work to identify what "all reasonable efforts" really means. The second question to be answered is equally relevant: "Is there currently a significant risk to public health and safety from dental radiography to merit extending the ALARA concept to the extent recommended by NCRP No. 145?"
To argue against extending ALARA to its ultimate limits appears somewhat like arguing against motherhood and apple pie. However, evidence will be presented to demonstrate that Report 145 provides a skewed analysis of present knowledge of radiation risks and radiation biology in order to justify their extreme interpretation of the ALARA principle. As we move into an era of "evidence based dentistry" governing methods of treatment, and decision making, we need to seriously ask: "What is the evidence supporting the need to implement all of the recommendations found in report No. 145 and does the evidence provided really require that all recommendations be followed to fulfill the principle of ALARA?"
Summary of Key Recommendations of NCRP Report No. 145, Radiation Protection in Dentistry
"Dentists shall use x-ray equipment and procedures in a manner that ensures compliance with both the recommendations in this report and the requirements of their state or political jurisdictions. When there are discrepancies between these recommendations and legal requirements, the more rigorous shall take precedence [p. 6]."
Impact on dentistry: Report No. 145 recommendations are currently "more rigorous" than most states and political jurisdictions, thus compliance with their recommendations would appear to be mandatory.
The Dentists Role in Radiation Protection
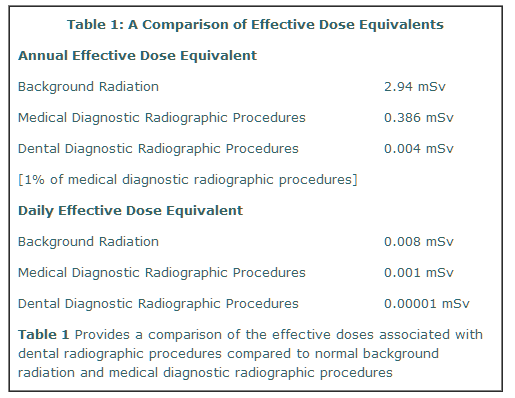
Report No. 145, figure 2.1, illustrates that the average annual effective dose equivalent to the U.S. population is 3.57 mSv. The concept of "effective dose" represents an estimate of the potential total body risk of developing cancer or genetic effects from a specified dose of radiation, regardless of whether the radiation is delivered to a local area or the whole body. Of the 3.57 mSv, 82% [2.94 mSv] is derived from "natural" sources called background radiation and an estimated 11% [0.39 mSv] derived from diagnostic "medical" exposures. Report No. 145 indicates that an estimated 1% of effective dose associated with diagnostic medical radiography may be attributed to dentistry [page 8]. The data therefore present two opportunities for comparing potential carcinogenic and genetic radiation risks as seen in Table 1 below.
In standard NCRP terminology, "shall and shall not" statements indicate adherence to the recommendation is necessary to meet accepted standards of protection; "should and should not" statements are used to indicate prudent practice. In classic understated fashion the report "makes a number of recommendations for the dentist" to achieve the reports defined ALARA goals. NCRP No. 145 then proceeds to make 64 "shall" recommendations, 24 "shall not" recommendations, 15 "should" and 6 "should not" recommendations [total 109], making this a highly prescriptive document, whose intent is almost guaranteed to radically change the way dental radiography is practiced on a daily basis. In contrast, the previous NCRP Report No. 35 only included 30 shall statements, 6 shall not statements and 22 should statements [total 58]
NCRP No. 145 clearly establishes the guidelines for "best practices" in dental radiography, as well as the ultimate extension of the ALARA concept to every facet of dental radiography. The report's recommendations will require dentistry and dental x-ray laboratories to evaluate how dental radiography is currently practiced and at the same time work to identify what "all reasonable efforts" really means. The second question to be answered is equally relevant: "Is there currently a significant risk to public health and safety from dental radiography to merit extending the ALARA concept to the extent recommended by NCRP No. 145?"
To argue against extending ALARA to its ultimate limits appears somewhat like arguing against motherhood and apple pie. However, evidence will be presented to demonstrate that Report 145 provides a skewed analysis of present knowledge of radiation risks and radiation biology in order to justify their extreme interpretation of the ALARA principle. As we move into an era of "evidence based dentistry" governing methods of treatment, and decision making, we need to seriously ask: "What is the evidence supporting the need to implement all of the recommendations found in report No. 145 and does the evidence provided really require that all recommendations be followed to fulfill the principle of ALARA?"
Summary of Key Recommendations of NCRP Report No. 145, Radiation Protection in Dentistry
"Dentists shall use x-ray equipment and procedures in a manner that ensures compliance with both the recommendations in this report and the requirements of their state or political jurisdictions. When there are discrepancies between these recommendations and legal requirements, the more rigorous shall take precedence [p. 6]."
Impact on dentistry: Report No. 145 recommendations are currently "more rigorous" than most states and political jurisdictions, thus compliance with their recommendations would appear to be mandatory.
The Dentists Role in Radiation Protection
- Shall establish a radiation protection program
- Shall seek guidance from a qualified expert
- Shall prescribe all radiographic examinations
- Shall conduct a clinical history and physical exam and determine health benefit to patient from the radiographic procedure
- Shall obtain guidance from a qualified expert [facility design & radiation protection
- Shall be qualified and credentialed to take radiograph
- Shall make an effort to obtain recent radiographs from patient's previous dentist
- Shall take radiographs only if indicated after an evaluation of clinical history, physical exam or laboratory findings
- Shall limit radiographic examinations of symptomatic patients to those required for diagnosis and treatment of current disease
- Shall not expose radiographs for administrative purposes
- X-ray equipment shall meet government standards
- X-ray units shall not have a kVp of less than 50 kVp or higher than 100 kVp
- Position Indicating Devices/cones shall be open ended and attenuate scattered radiation
- Source to image receptor distance shall not be less than 20 cm (8")
- Rectangular collimation shall be routinely used for periapical radiography
- Shall not use image receptors slower than ANSI speed group E
- Occupationally exposed personnel shall not restrain uncooperative patients. Public who restrain patients or hold image receptors during exposure shall be provided with shielding, e.g. lead aprons, gloves
- Shall use fastest imaging system consistent with imaging task
- Shall use high speed [400 or greater] rare-earth screen-film systems
- Shall use high speed [400 or greater] rare-earth screen-film systems or digital systems of equivalent or greater speed
- Shall use fastest screen-film systems compatible with imaging requirements
- Shall place soft tissue/profile filters at x-ray source NOT image receptor
- Shall collimate beam to area of clinical interest
- Shall use time-temperature processing or equivalent
- Shall not use sight development
- Shall use minimum patient dose
- For maximum diagnostic yield: quiet atmosphere, free from distractions, masked viewbox, opaque film mounts, variable illumination viewbox, reduced room lighting, use a magnifier
- Shall not be required if all NCRP 145 recommendations are rigorously followed
- Shall provide thyroid collars for children
- New and remodeled dental facilities shall be designed by a qualified expert
- Shielding shall be increased if conventional building structure is inadequate
- Shielding shall be determined by calculation and survey measurements
- New offices shall provide protective barriers for operators
- Barriers shall maintain visual contact and communication with patients
- In the absence of barriers the operator shall remain 2 meters [6 feet 8 inches] from tubehead during exposure
- If the operator cannot stand 2 meters [6 feet 8 inches] from tubehead a barrier shall be provided
- Shall be provided for known pregnant-occupationally exposed personnel
- Shall treat a patient in a room during diagnostic exposure as a member of the public
- Shall design new dental facilities so that public will not receive in excess of 1 mSv annually
- Shall develop a written protocol for periodic quality assurance for each x-ray machine, image receptor system, and processor or darkroom
- Shall have a radiation protection survey for each new dental x-ray installation
- Shall perform resurveys of x-ray units no less than once every four years
- Shall resurvey x-ray units after any change in the installation, workload, or operating conditions that might significantly increase occupational exposure or public exposure
- Shall evaluate daily: darkroom chemistry and processor
- Shall evaluate each type of film for fog and artifacts monthly and each time a new box or batch of film is opened
- Shall discard or return to vendor excessively fogged film
- Shall visually evaluate screen-film cassettes after any accident, or at 6 month intervals
- Shall replace or repair defective screen-film cassettes
- Shall evaluate each darkroom and daylight loader monthly
- Shall visually inspect leaded aprons and thyroid collars monthly for defects
- Shall maintain a log of all Quality Assurance procedures. The log shall contain: date, procedure, results & corrective action if any
- Dentist shall provide training in radiation protection for all dental personnel
- This section of Report No. 145 includes 14 shall, 1 should not, 2 should, 2 should not statements and will not be enumerated
- Dental facilities, x-ray equipment performance and operating procedures should be established to maintain patient, occupational and public exposures as low as reasonably achievable, economic and social factors being taken into account [the ALARA principle].
- Dentist should use selection criteria to determine the extent of radiographic examination of asymptomatic patients
- X-ray equipment should conform to international standards
- kVp of x-ray units should not be less than 60 kVp
- kVp of x-ray units should not be more than 80 kVp
- Source to image receptor distance should not be less than 40 cm [16"]
- The rectangular beam should not exceed the dimensions of the image receptor by more than 2% of the source-to-image receptor distance
- A rectangular beam should be used for interproximal radiography when feasible
- Should use a lead apron IF NCRP No. 145 recommendations are not implemented
- Should provide a thyroid collar for adults when it will not interfere with radiographic procedures
- Personal dosimeters should be provided if personnel are likely to receive an effective dose of 1 mSv annually
- Should perform a fluoroscopic examination of lead aprons and thyroid collars annually
- Accrediting agencies should re-examine adequacy of their criteria for undergraduate education.
- Dentist and Auxiliaries should regularly attend continuing education courses in dental radiology and radiation protection
Report No. 145, figure 2.1, illustrates that the average annual effective dose equivalent to the U.S. population is 3.57 mSv. The concept of "effective dose" represents an estimate of the potential total body risk of developing cancer or genetic effects from a specified dose of radiation, regardless of whether the radiation is delivered to a local area or the whole body. Of the 3.57 mSv, 82% [2.94 mSv] is derived from "natural" sources called background radiation and an estimated 11% [0.39 mSv] derived from diagnostic "medical" exposures. Report No. 145 indicates that an estimated 1% of effective dose associated with diagnostic medical radiography may be attributed to dentistry [page 8]. The data therefore present two opportunities for comparing potential carcinogenic and genetic radiation risks as seen in Table 1 below.
From the above data, if one attempts to use estimated "average annual doses" from all sources as an estimate of potential cancer and genetic harm, dental diagnostic radiation exposures are 97- 100X lower than medical diagnostic procedures and 735 - 800X lower than background. NCRP No. 145 concludes based upon the above: "Thus, dental radiation is a minor contributor to total population burden. However, appropriate measures are necessary to maintain dental radiation exposures ALARA." [NCRP, No. 145, p8] Based upon its own evidence, NCRP figure 2.1 provides direct evidence that dental radiographic exposures do not present a public health risk of any significant merit and that dentistry may already be using sufficiently "appropriate measures" to keep public health risks well below those of other sources of population exposure, e.g., medical diagnostic, medical nuclear medicine and consumer product exposures.
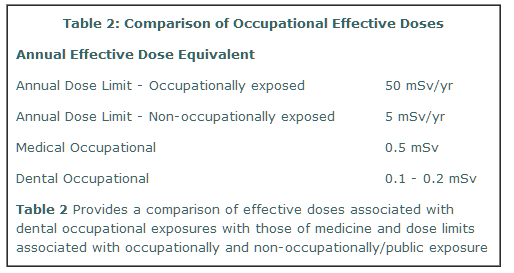
NCRP No. 145 presents current occupational exposure guidelines and data in their Figure 2.2 showing a continuous decline in occupational effective doses from 1960 through 1995 with U.S. occupational doses at 0.1 mSv/yr; while their Table 2.1 indicates 0.2 mSv/yr. The report concludes: "In dentistry, the application of the ALARA principle is expected to reduce effective doses to individuals well below the applicable dose limits." Table 2 below summarizes current estimates of effective doses to occupationally exposed persons for both medicine and dentistry [NCRP, No. 145, p10-11].
NCRP No. 145 presents current occupational exposure guidelines and data in their Figure 2.2 showing a continuous decline in occupational effective doses from 1960 through 1995 with U.S. occupational doses at 0.1 mSv/yr; while their Table 2.1 indicates 0.2 mSv/yr. The report concludes: "In dentistry, the application of the ALARA principle is expected to reduce effective doses to individuals well below the applicable dose limits." Table 2 below summarizes current estimates of effective doses to occupationally exposed persons for both medicine and dentistry [NCRP, No. 145, p10-11].
Evidence presented in NCRP No. 145 indicates that dental occupational exposures are approximately 250X to 500X lower than currently established Annual Dose Limits and 25X to 50X lower than present Nonoccupational/ Public dose limits and 5X lower than our colleagues in the healing arts and 29X lower than annual background radiation. The evidence suggests that at 250- 500X less than present annual dose limits for occupationally exposed persons, dentistry already appears to be "well below acceptable dose limits." Yet, NCRP Report No. 145 makes the following recommendation: "The dentist...shall establish a radiation protection program as outlined above. The dentist shall seek guidance of a qualified expert in this activity." The radiation protection program the report describes consists of seven specific activities to be performed by the dentist/radiation safety officer. No evidence is provided to demonstrate why a qualified expert with special expertise is required. The seven elements of the proposed radiation protection program are well identified in the report. The special guidance of the qualified expert could easily be performed by consulting an appropriate journal article, or by participation in a continuing education course.
Three of the biggest recommendations for "change" promoted in NCRP, No. 145 are their recommendations that: 1) dentists shall not use any film or digital imaging system slower than ANSI Speed Group E films for intraoral radiography, 2) shall use rectangular collimation, and 3) shall use high-speed [400 or greater] rare earth screen-film systems, or digital-imaging systems of equivalent or greater speed. Of all of the reports recommendations, these three elements have the potential to reduce patient somatic [cheek & head] exposures by at least 50% if E/F film is used, 45-95% [depending on anatomic location] if rectangular collimation is used and 75% if the faster screen-film combinations are used for panoramic and cephalometric radiographs instead of slower 100 speed screen-film combinations. It is because of these significant somatic dose reductions, along with the corresponding reduction in scattered radiation, that the report indicates that the lead apron will no longer be required to prevent reproductive organ exposure. All three recommendations are very attractive applications of the ALARA principle; the reduction in somatic exposure to the patient is clearly a major benefit, and there is clearly a reduction in the effective dose equivalent to the individual patient. However, the overall public health benefit of these three recommendations, in terms of additional reduced cancers, genetic defects, etc. derivable from applying these concepts is less clear.
The dental effective dose equivalent to patients, as presented in Table 1, indicates that dentistry's effective dose equivalent is already 735 - 800X lower than background. The expected reduction in patient dose, if the recommendations proposed in the report are implemented, requires asking the question: "Is there evidence to demonstrate that a further reduction in dental effective dose equivalent from the present 800X down to >1600X lower than background will have a measurable effect on the public health of U.S. citizens?" Are we not already at a level of population exposure where we can say 50% - 80% of "nothing" is still nothing? NCRP Report No. 1214 states: "...for radiation protection purposes, it is prudent to assume the effect per unit dose in the low-dose region following single acute exposures or lowdose fractions is a linear response... Genetic effects may result from a gene mutation, or a chromosome aberration...It is conceptually possible, but with a vanishingly small probability, [emphasis mine] that any of these effects could result from the passage of a single charged particle, causing damage to DNA that could be expressed as a mutation or small deletion..." The evidence would suggest that at 800X lower than background radiation we are already within the "vanishingly small probability" realm.
The recommendation relating to rectangular collimation specifically includes a "shall" statement for periapical radiographs but leaves the use of rectangular collimation for interproximal/bitewing radiographs at the discretion of the clinician.
As an indication of prudent practice, Report No. 145 recommends that for the rectangular collimating device: "Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimension of the image receptor by more than two percent of the source-to-image receptor distance." The impact of this recommendation will significantly influence the practice of dental radiography because it would potentially require the use of a separate BID for each size film used in the practice or use a specific device made by a limited number of manufacturers. Strict enforcement of the 2% source-image receptor distance would create a situation where the dentist would have to purchase separate BID's, or beam collimating image receptor holders for each size image receptor used in the office. Is it really practical, and necessary from a public health perspective, to require such restrictive limitation of the beam of radiation simply to extend the concept of ALARA? Where is the evidence to demonstrate a meritorious reduction in cancer and genetic risk sufficient to justify the recommendation other than it produces a lower somatic and effective dose?
In implementing a rather draconian extension of the ALARA concept to the practice of dental radiography, Report No. 145 has chosen to ignore two previous NCRP Reports 6,7, No. 91 and No. 93. Report No. 91 establishes the concept of the Negligible Individual Risk Level [NIRL]. NIRL is defined as a "level of average annual excess risk of fatal health effects attributable to irradiation, below which further effort to reduce radiation exposure to the individual is unwarranted. The NIRL is regarded as trivial compared to the risk of fatality associated with ordinary, normal societal activities and can, therefore, be dismissed from consideration...Such levels, at or below the NIRL, are not required to be considered for purposes of radiation protection...THE NIRL is regarded as a threshold below which the control of radiation sources and limitation of exposures, i.e., efforts to reduce risk further would be deliberately and specifically curtailed [emphasis mine]", p 43.
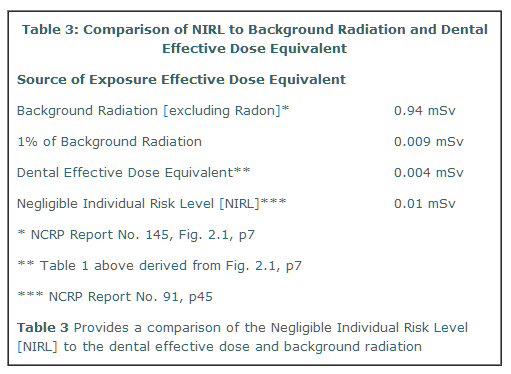
Report No. 91 also states that "In the radiation protection field, the need for a reasonably negligible risk level to avoid excessive control actions and expenditures to reduce individual risk has long been recognized", p. 44. Report 91 then identifies six criteria relevant to gage the smallness or triviality of risk which when considered together offer degrees of reasonableness and perspective that "tend to minimize subjective aspects of judgment". "Smallness of risk is considered in relation to: 1) magnitude of dose, 2) difficulty in detection and measurement of dose and health effect, 3) natural risk for the same health effects, 4) estimated risk for the mean and variance of natural background radiation exposure levels, 5) risks to which people are accustomed; and 6) perception of and behavioral response to risk levels," p. 44. The NIRL is established as an annual dose equivalent increment of about 0.01 mSv which is about 1% of the average natural background radiation exposure excluding radon for continuous or repeated exposure. Table 3 compares the NIRL to background and dental average effective dose equivalent.
Three of the biggest recommendations for "change" promoted in NCRP, No. 145 are their recommendations that: 1) dentists shall not use any film or digital imaging system slower than ANSI Speed Group E films for intraoral radiography, 2) shall use rectangular collimation, and 3) shall use high-speed [400 or greater] rare earth screen-film systems, or digital-imaging systems of equivalent or greater speed. Of all of the reports recommendations, these three elements have the potential to reduce patient somatic [cheek & head] exposures by at least 50% if E/F film is used, 45-95% [depending on anatomic location] if rectangular collimation is used and 75% if the faster screen-film combinations are used for panoramic and cephalometric radiographs instead of slower 100 speed screen-film combinations. It is because of these significant somatic dose reductions, along with the corresponding reduction in scattered radiation, that the report indicates that the lead apron will no longer be required to prevent reproductive organ exposure. All three recommendations are very attractive applications of the ALARA principle; the reduction in somatic exposure to the patient is clearly a major benefit, and there is clearly a reduction in the effective dose equivalent to the individual patient. However, the overall public health benefit of these three recommendations, in terms of additional reduced cancers, genetic defects, etc. derivable from applying these concepts is less clear.
The dental effective dose equivalent to patients, as presented in Table 1, indicates that dentistry's effective dose equivalent is already 735 - 800X lower than background. The expected reduction in patient dose, if the recommendations proposed in the report are implemented, requires asking the question: "Is there evidence to demonstrate that a further reduction in dental effective dose equivalent from the present 800X down to >1600X lower than background will have a measurable effect on the public health of U.S. citizens?" Are we not already at a level of population exposure where we can say 50% - 80% of "nothing" is still nothing? NCRP Report No. 1214 states: "...for radiation protection purposes, it is prudent to assume the effect per unit dose in the low-dose region following single acute exposures or lowdose fractions is a linear response... Genetic effects may result from a gene mutation, or a chromosome aberration...It is conceptually possible, but with a vanishingly small probability, [emphasis mine] that any of these effects could result from the passage of a single charged particle, causing damage to DNA that could be expressed as a mutation or small deletion..." The evidence would suggest that at 800X lower than background radiation we are already within the "vanishingly small probability" realm.
The recommendation relating to rectangular collimation specifically includes a "shall" statement for periapical radiographs but leaves the use of rectangular collimation for interproximal/bitewing radiographs at the discretion of the clinician.
As an indication of prudent practice, Report No. 145 recommends that for the rectangular collimating device: "Each dimension of the beam, measured in the plane of the image receptor, should not exceed the dimension of the image receptor by more than two percent of the source-to-image receptor distance." The impact of this recommendation will significantly influence the practice of dental radiography because it would potentially require the use of a separate BID for each size film used in the practice or use a specific device made by a limited number of manufacturers. Strict enforcement of the 2% source-image receptor distance would create a situation where the dentist would have to purchase separate BID's, or beam collimating image receptor holders for each size image receptor used in the office. Is it really practical, and necessary from a public health perspective, to require such restrictive limitation of the beam of radiation simply to extend the concept of ALARA? Where is the evidence to demonstrate a meritorious reduction in cancer and genetic risk sufficient to justify the recommendation other than it produces a lower somatic and effective dose?
In implementing a rather draconian extension of the ALARA concept to the practice of dental radiography, Report No. 145 has chosen to ignore two previous NCRP Reports 6,7, No. 91 and No. 93. Report No. 91 establishes the concept of the Negligible Individual Risk Level [NIRL]. NIRL is defined as a "level of average annual excess risk of fatal health effects attributable to irradiation, below which further effort to reduce radiation exposure to the individual is unwarranted. The NIRL is regarded as trivial compared to the risk of fatality associated with ordinary, normal societal activities and can, therefore, be dismissed from consideration...Such levels, at or below the NIRL, are not required to be considered for purposes of radiation protection...THE NIRL is regarded as a threshold below which the control of radiation sources and limitation of exposures, i.e., efforts to reduce risk further would be deliberately and specifically curtailed [emphasis mine]", p 43.
Report No. 91 also states that "In the radiation protection field, the need for a reasonably negligible risk level to avoid excessive control actions and expenditures to reduce individual risk has long been recognized", p. 44. Report 91 then identifies six criteria relevant to gage the smallness or triviality of risk which when considered together offer degrees of reasonableness and perspective that "tend to minimize subjective aspects of judgment". "Smallness of risk is considered in relation to: 1) magnitude of dose, 2) difficulty in detection and measurement of dose and health effect, 3) natural risk for the same health effects, 4) estimated risk for the mean and variance of natural background radiation exposure levels, 5) risks to which people are accustomed; and 6) perception of and behavioral response to risk levels," p. 44. The NIRL is established as an annual dose equivalent increment of about 0.01 mSv which is about 1% of the average natural background radiation exposure excluding radon for continuous or repeated exposure. Table 3 compares the NIRL to background and dental average effective dose equivalent.
Table 3 shows that the current estimated public health risk/detriment to the U.S. public from dental diagnostic radiographic procedures is about 2.5X lower than the NIRL. NCRP Report No. 93 subsequently recognizes the "trivial" nature of the dental effective dose equivalent in contributing to calculating a "collective effective dose equivalent" [a measure of the radiation detriment to the entire U.S. population] by stating: "Dental examinations have been omitted since they are estimated to contribute less than 0.01 mSv (1 mrem) to the total average annual effective dose equivalent," p 46.
NCRP No. 145 presents two selective and incomplete citations from available literature to imply a stronger association between the risk of specific cancers and dental radiographic exposures than the actual data merits. Specifically: "A few epidemiological studies have demonstrated statistically-significant associations between dental x-ray exposure and cancer (e.g., Graham et al., 1966; Preston-Martin et al., 1988)", p 45) and "Epidemiological studies have shown associations between diagnostic exposure (including dental) and leukemia (Graham et al., 1966, p 58)", and "An association of both brain and meningeal tumors with dental x-ray has been identified, but statistical significance is marginal (Preston- Martin et al., 1989", p61). The Graham et al.8, reference actually reported NO association with cancer [leukemia] and dental radiographs when considered as a separate element. "The risks for individuals receiving radiation to the chest only, extremities only, and teeth only revealed nothing of interest, Table 16," [p. 364]. It was only when dental x-rays were combined with "other x-ray procedures" that a statistically significant association was identified among children 6 months to 12 months of age. In the Graham et al article, the relative risk from dental exposure alone was 1.38 & 1.42 and not statistically significant; when radiographic exposure to "other sites" were added, the relative risk rose to statistical significance at 3.2 & 2.8 for the two groups of children studied. The Preston-Martin et al9, 10, statistically significant association between dental radiographs and parotid cancer only occurred at levels of parotid doses of 0.5 Gy and higher attributable to exposures during the 1920's to 1940's when beams were poorly filtered and collimated and film speeds very slow, resulting in high patient doses. There was no statistically significant correlation with either malignant or benign parotid tumors at doses lower than 0.5 Gy. Both Preston-Martin et al studies lack modern era credibility because they point to risks associated with levels of exposure easily 90X to 5,000X larger than parotid doses from today's dental radiographic procedures.
NCRP Report 145's Appendix B, "Risk Assessment" includes a detailed evaluation of stochastic and deterministic radiation effects to major organ systems associated with high doses of radiation. A nice feature of this appendix is that at the end of each topic, the specific contribution of dental radiography to the organ is presented in such a way that it is easy for the reader to compare the low dental dose with the minimum dose associated with the risk of detrimental effects. In every instance the dental dose is reported as being well below [182X to 200,000X lower] the minimum dose associated with detrimental effects as expressed in %risk/Sv.
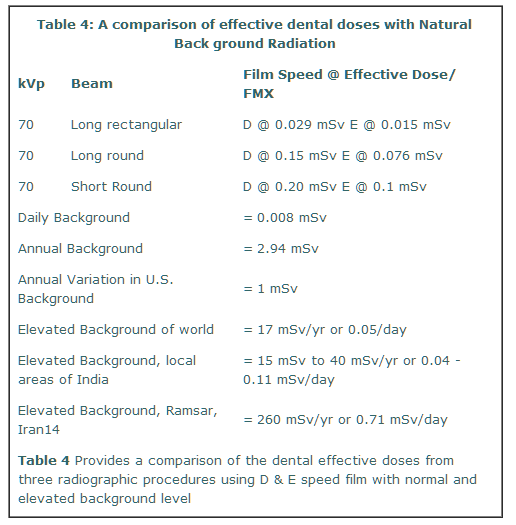
Throughout NCRP Report No. 145 there is an ever-present theme presented relating to the uncertainty of potential radiation risks associated with the low levels of dental diagnostic radiographic procedures necessitating that all of the report's ALARA recommendations be followed. The report fails to include any significant arguments or comparisons to suggest that present effective doses from dentistry may not actually place patients at any additional risk for developing detrimental effects of any kind. For example, Billen11 estimates that there are about 8,000 "spontaneous DNA lesions" created by thermal and oxidative insult every hour, or roughly 70,000,000 per year! Billen points out that intra-nuclear repair processes completely repair this damage without difficulty. He estimates that a 10 mSv absorbed dose would create an additional 100 DNA damaging events. We can compare this estimate of 100 "extra" DNA damaging events for a 10 mSv absorbed dose with NCRP Report No. 145's Table 6.1 showing the highest effective dose using D speed film and long round BID to be 0.15 mSv or about 1.5 potential DNA damaging events per cell per full mouth radiographic survey in contrast to the 8,000 spontaneous lesions. Additionally, there is no mention of the fact that there are large populations living in areas of high natural background radiation averaging about 17 mSv/year12, with an upper range of 40 mSv to 260 mSv13, 14. These high natural background radiation exposed populations exhibit no significant increase in radiation detriment with a level of background from 5.8X to 13.6X greater than the U.S. An effective dose of 0.15 mSv from a full mouth survey, therefore becomes 113X to 267X LOWER than the dose to individuals residing in areas of high natural background radiation. Table 4 provides a comparison of these radiation levels.
NCRP No. 145 presents two selective and incomplete citations from available literature to imply a stronger association between the risk of specific cancers and dental radiographic exposures than the actual data merits. Specifically: "A few epidemiological studies have demonstrated statistically-significant associations between dental x-ray exposure and cancer (e.g., Graham et al., 1966; Preston-Martin et al., 1988)", p 45) and "Epidemiological studies have shown associations between diagnostic exposure (including dental) and leukemia (Graham et al., 1966, p 58)", and "An association of both brain and meningeal tumors with dental x-ray has been identified, but statistical significance is marginal (Preston- Martin et al., 1989", p61). The Graham et al.8, reference actually reported NO association with cancer [leukemia] and dental radiographs when considered as a separate element. "The risks for individuals receiving radiation to the chest only, extremities only, and teeth only revealed nothing of interest, Table 16," [p. 364]. It was only when dental x-rays were combined with "other x-ray procedures" that a statistically significant association was identified among children 6 months to 12 months of age. In the Graham et al article, the relative risk from dental exposure alone was 1.38 & 1.42 and not statistically significant; when radiographic exposure to "other sites" were added, the relative risk rose to statistical significance at 3.2 & 2.8 for the two groups of children studied. The Preston-Martin et al9, 10, statistically significant association between dental radiographs and parotid cancer only occurred at levels of parotid doses of 0.5 Gy and higher attributable to exposures during the 1920's to 1940's when beams were poorly filtered and collimated and film speeds very slow, resulting in high patient doses. There was no statistically significant correlation with either malignant or benign parotid tumors at doses lower than 0.5 Gy. Both Preston-Martin et al studies lack modern era credibility because they point to risks associated with levels of exposure easily 90X to 5,000X larger than parotid doses from today's dental radiographic procedures.
NCRP Report 145's Appendix B, "Risk Assessment" includes a detailed evaluation of stochastic and deterministic radiation effects to major organ systems associated with high doses of radiation. A nice feature of this appendix is that at the end of each topic, the specific contribution of dental radiography to the organ is presented in such a way that it is easy for the reader to compare the low dental dose with the minimum dose associated with the risk of detrimental effects. In every instance the dental dose is reported as being well below [182X to 200,000X lower] the minimum dose associated with detrimental effects as expressed in %risk/Sv.
Throughout NCRP Report No. 145 there is an ever-present theme presented relating to the uncertainty of potential radiation risks associated with the low levels of dental diagnostic radiographic procedures necessitating that all of the report's ALARA recommendations be followed. The report fails to include any significant arguments or comparisons to suggest that present effective doses from dentistry may not actually place patients at any additional risk for developing detrimental effects of any kind. For example, Billen11 estimates that there are about 8,000 "spontaneous DNA lesions" created by thermal and oxidative insult every hour, or roughly 70,000,000 per year! Billen points out that intra-nuclear repair processes completely repair this damage without difficulty. He estimates that a 10 mSv absorbed dose would create an additional 100 DNA damaging events. We can compare this estimate of 100 "extra" DNA damaging events for a 10 mSv absorbed dose with NCRP Report No. 145's Table 6.1 showing the highest effective dose using D speed film and long round BID to be 0.15 mSv or about 1.5 potential DNA damaging events per cell per full mouth radiographic survey in contrast to the 8,000 spontaneous lesions. Additionally, there is no mention of the fact that there are large populations living in areas of high natural background radiation averaging about 17 mSv/year12, with an upper range of 40 mSv to 260 mSv13, 14. These high natural background radiation exposed populations exhibit no significant increase in radiation detriment with a level of background from 5.8X to 13.6X greater than the U.S. An effective dose of 0.15 mSv from a full mouth survey, therefore becomes 113X to 267X LOWER than the dose to individuals residing in areas of high natural background radiation. Table 4 provides a comparison of these radiation levels.
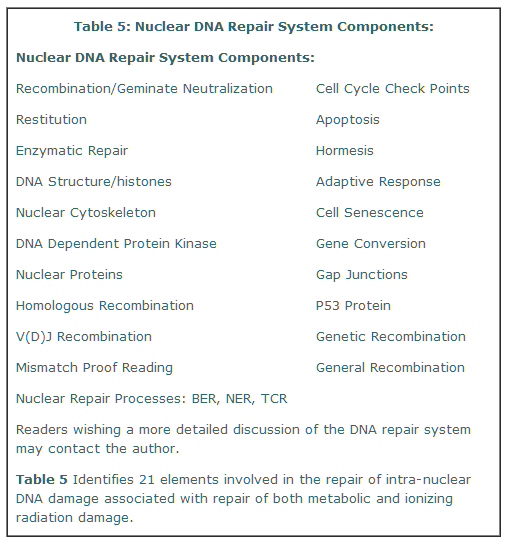
NCRP Report No. 145 fails completely by omission to provide any discussion whatsoever relating to the vast array of literature relating to intra-nuclear DNA repair processes referred to by Dr. Myron Polycove15 as the "DNA damage-control biosystem." This DNA repair system is physiologically operative on both metabolic and radiation damage produced by free radicals and is directly relevant to the potential reduction in risk to patients regarding their somatic exposure [cheek/head radiation] and total body detriment as described by the effective dose [total body genetic/ cancer risks]. Polycove further points out that the public policy sector, such as the NCRP and ICRP, etc., focus on the damage potentially caused by low-level radiation without taking into consideration the effectiveness of the DNA damage-control biosystem. It is not within the scope of this article to elaborate on the cell's DNA repair system, but some of the major elements in the process are summarized in Table 5 below.
NCRP Report No. 145 has chosen to perpetuate the concept of endless extrapolation of radiation risks from high levels of exposure down to the very small doses associated with patient exposure to dental diagnostic exposures and dental occupational exposures. The report consistently cites the "uncertainty of risks" associated with low doses of radiation exposure, without seriously considering an alternative hypothesis, i.e., that all dental radiation risks are currently so low that further consideration to reducing them may not be justified. For example, Hofman and Katz16 estimate the statistical probability of 10 mSv of low-LET radiations inducing cancer is about 10-15, or one chance in a million billion! For anatomic structures like the thyroid gland receiving about 0.4 mSv/FMX, the statistical probability for thyroid cancer would be one chance in about 100 million billion. Walinder17has concluded: "In recent years, we have obtained a growing insight that the difference between them [normal and cancer cells] is not an either-or effect but rather a quantitative one, and that the formation of a cancer cell, as well as its development to a macroscopic tumor, depends on a series of unpredictable events which occur within a heterogeneous human population." Trosko18 suggests that cancer consists of as many as five or more discrete steps and that low level ionizing radiation exposures are currently viewed as "a rather poor 'initiator and complete carcinogen', but may be an effective 'progressor' by being a 'deletion mutagen.'" Trosko further concludes that: "The old dogma of 'radiation causes cancer' has been replaced with the concept that there is 'no single cause of cancer...it will be extremely difficult to assign 'causation' by low level ionizing radiation, and since 'cancer is not 'caused' by just one thing, i.e., radiation, one must be very cautious in attributing any 'excess' cancers to the 'one thing' or radiation."
NCRP Report No. 145 makes a valiant, if not schizophrenic, attempt to walk a tightrope of using the uncertainty of low dose radiation risks to assert the extension of the ALARA principle while at the same time clearly making statements intended to down-play the risks. Such statements include, but are not limited to the following: "However, it is not clear that radiation in doses required for dental radiography presents any risk. Neither is it clear that these small doses are free of risk." [p.1] "Actual fatal cancer risk for radiation may be more, less, or even zero". [p.5] "These data suggest that dental personnel are not expected to receive occupational exposures greater than the recommended threshold for monitoring of 1 mSv/yr." [p.29] "There is no conclusive proof that the radiation exposure from [dental] x-rays is harmful." [p.45] "If a substantial risk existed it would have been identified and reported. It seems reasonable to conclude that radiation related risks to dental patients and dental x-ray equipment operators are numerically very small and may be zero." [p45] "These doses are much smaller than the minimum doses for which coefficients of risk per unit dose can be meaningfully applied. They are numerically equal to the unavoidable natural environmental exposure received in a few hours to a few days by the average American." [p. 45]
NCRP Report No. 145 suggests that dentist's should perform fluoroscopic examination of their lead aprons annually. The evidence supporting this recommendation as a prudent practice is not specified, other than the fear that cracks might appear which could allow miniscule amounts of scattered radiation to penetrate the lap area in random locations. Such a suggestion might be appropriate for the old leaded aprons made from lead impregnated rubber which were brittle and could not be folded without fear of developing stress fractures; however, modern leaded aprons constructed from multiple layers of flexible lead impregnated vinyl should make fluoroscopic examination annually irrelevant and unnecessary for dentistry.
NCRP Report No. 145 states in the introduction: "Office design, equipment, and procedures that minimize patient exposure will also reduce exposure to the operator and the public. Additional measures, however, may be required to ensure that doses to operators and the public are within limits established by regulatory bodies. Doses to all should be kept as low as reasonably achievable, with economic and social factors being taken into account (i.e., the ALARA Principle) (NCRP, 1990)." (p1). The U.S. Dept. of Energy states20: "The ALARA process is a decision-making tool with the goal to maximize the total benefits of the radiological protection provisions for the DOE activity that is likely to expose members of the public to ionizing radiation. This occurs when the cost of radiological protection plus the cost of the detriment are minimal. The procedure for attaining the minimal cost condition is called "optimization." The acceptable cost to reduce the collective dose to a population of exposed persons falls within a range of $500 to $2,500 per personrem21 [1 rem = 10 mSv]. The collective effective dose from dental radiographic procedures is presently estimated to be 0.004 mSv/yr. The expenditure of $500 to $2,500 to reduce the collective dose that is presently 735X lower than annual background radiation levels; and 2,500X lower than the 10 mSv collective dose reduction goal is clearly unjustifiable by the imaginary and immeasurable gain in potential benefit.
NCRP Report No. 145 emphasizes the desirability of incorporating a more consistent and strict application of radiographic selection criteria and the incorporation of certain quality assurance procedures, the use of faster image receptors, timetemperature processing, proper interpretation strategies. Such recommendations have merit and certainly deserve appropriate consideration for incorporation into the practice to reduce patient exposures and maintain the highest diagnostic quality radiographs.
Conclusions:
This paper attempts to analyze some of the factual information presented in NCRP Report No. 145, and compares this data in ways that clearly place the public health and occupational risks associated with dental radiography into a clear perspective through comparison of the reported doses attributable to patient and occupational exposures in dentistry with current dose limits and background radiation. In every instance, the effective dose to patients and occupational exposures are many, many times lower than background or the relevant dose limits governing occupational and public exposure. This paper also discusses specific recommendations from Report No. 145 which appear to lack credible supporting evidence, or a significant failure to perceive the impact of their own recommendation; examples include fluoroscopy of lead aprons annually and the specification that rectangular collimated beams not exceed source to image receptor distances by 2% resulting in the potential to have a separate BID or rectangular beam collimating film holder set for each image receptor size in use.
There are several positive benefits to be derived from incorporating some of the reports recommendations into dental radiography practices that should be emphasized. The consistent application of radiographic selection criteria in the prescription of radiographic examinations, the use of faster image receptors and screen/film combinations, along with closer attention to principles of radiographic quality assurance will provide dentists with high quality diagnostic images along with reduced patient dose.
Data provided in Report No. 145 is used as evidence to indicate that dental radiography in the U.S. is already ALARA and that the expenditure of additional financial resources to achieve an even greater level of ALARA is probably unjustified and unmerited since present risks are already immeasurable, undetectable and do not jeopardize the public health. Indeed, two previous NCRP reports have already drawn this conclusion: NCRP Report 107: "It is tempting to conclude that further occupational exposure reduction in dentistry may not be cost-effective." NCRP Report 93 recognizes the "trivial" nature of the dental effective dose equivalent in contributing to calculating a collective effective dose equivalent by stating: "Dental examinations have been omitted since they are estimated to contribute less than 0.01 mSv (1 mrem) to the total average annual effective dose equivalent."
The scientific principle used to under gird NCRP Report No. 145 is the assumption that radiation risks may be extrapolated indefinitely in a linear fashion from high doses to very low doses, the linear nonthreshold theory [LNT]. Polycove15 cites Dr. L.S. Taylor, past president of the National Council on Radiation Protection, as describing the linear extrapolation from high doses to very low doses in the calculation of collective doses as: "deeply immoral uses of our scientific heritage" [p366]. Bond, et al22 writing in opposition to the LNT: "The above arguments also appear to have destroyed rather completely the interpretations of and impressions from the linear hypothesis - that 'low level' irradiation should be of major personal or public health concern, a factor that has induced an almost pathological fear of low level irradiation in a major segment of the general population...It appears to be more sophistry than science, and reminiscent of the 'angels on the head of a pin' debates, to argue about whether a small amount of radiation energy can cause an excess malignancy... one excess cancer can not affect significantly a public health problem of the magnitude of cancer." Additionally, Kellerer and Nekolla22 appear to make a plea for a common sense approach to low dose radiation risk estimation when they state: "There is however, less agreement on the potential health effects of small doses. Such effects cannot be assessed in epidemiological investigations, nor can they be reliably inferred from cell studies or animal experiments... Speculative as such unobservable phenomena are, they cannot be ruled out - but common sense can ignore them." Abel Gonzalez23, as recently as Sept. 2004 has stated: "For purposes of radiation protection, however, the non-threshold concept at doses below background doses is not relevant. It is applicable only for doses above the prevalent background dose that is unavoidably incurred... Therefore, the discussion on whether smaller absolute dose, say some microsievert per year, would be able to induce health effects, or whether the dose-response relationship is LNT at such small doses is an interesting academic question but meaningless for practical radiation protection purposes."
Finally, NCRP Report No. 145 represents an "advisory opinion" on minimizing radiation risks to patients, the dentist and dental staff from dental diagnostic radiographic procedures. NCRP Reports are frequently used by various federal and state entities to establish rules and regulations; as a result it is critically important for dentists and dental x-ray technicians to understand what the NCRP has recommended for the practice of dental radiography because many of the 109 recommendations could, in the near future, become regulations and laws. Report No. 145 clearly places each dentist and x-ray technician, laboratory at a crossroad for decision-making. Every dentist and dental x-ray laboratory is encouraged to obtain a copy of the report and along with the information presented in this paper decide to either support, or not support, the incorporation of Report No. 145's many recommendations into State, Federal, OSHA, EPA and DOE regulations governing the practice of dental radiography. If you support the document's recommendations, then work actively for their incorporation into your State's practice act. On the other hand, if you do not support incorporating some or all of the recommendations in your State, then be vigilant and work with your legislative and State Board representatives and public health officials to see that they are not incorporated into the rules and regulations governing the practice of dental radiography. A failure to act on your convictions will permit someone else to decide how you will practice dental radiography in the future. The choice is ours.
NCRP Report No. 145 makes a valiant, if not schizophrenic, attempt to walk a tightrope of using the uncertainty of low dose radiation risks to assert the extension of the ALARA principle while at the same time clearly making statements intended to down-play the risks. Such statements include, but are not limited to the following: "However, it is not clear that radiation in doses required for dental radiography presents any risk. Neither is it clear that these small doses are free of risk." [p.1] "Actual fatal cancer risk for radiation may be more, less, or even zero". [p.5] "These data suggest that dental personnel are not expected to receive occupational exposures greater than the recommended threshold for monitoring of 1 mSv/yr." [p.29] "There is no conclusive proof that the radiation exposure from [dental] x-rays is harmful." [p.45] "If a substantial risk existed it would have been identified and reported. It seems reasonable to conclude that radiation related risks to dental patients and dental x-ray equipment operators are numerically very small and may be zero." [p45] "These doses are much smaller than the minimum doses for which coefficients of risk per unit dose can be meaningfully applied. They are numerically equal to the unavoidable natural environmental exposure received in a few hours to a few days by the average American." [p. 45]
NCRP Report No. 145 suggests that dentist's should perform fluoroscopic examination of their lead aprons annually. The evidence supporting this recommendation as a prudent practice is not specified, other than the fear that cracks might appear which could allow miniscule amounts of scattered radiation to penetrate the lap area in random locations. Such a suggestion might be appropriate for the old leaded aprons made from lead impregnated rubber which were brittle and could not be folded without fear of developing stress fractures; however, modern leaded aprons constructed from multiple layers of flexible lead impregnated vinyl should make fluoroscopic examination annually irrelevant and unnecessary for dentistry.
NCRP Report No. 145 states in the introduction: "Office design, equipment, and procedures that minimize patient exposure will also reduce exposure to the operator and the public. Additional measures, however, may be required to ensure that doses to operators and the public are within limits established by regulatory bodies. Doses to all should be kept as low as reasonably achievable, with economic and social factors being taken into account (i.e., the ALARA Principle) (NCRP, 1990)." (p1). The U.S. Dept. of Energy states20: "The ALARA process is a decision-making tool with the goal to maximize the total benefits of the radiological protection provisions for the DOE activity that is likely to expose members of the public to ionizing radiation. This occurs when the cost of radiological protection plus the cost of the detriment are minimal. The procedure for attaining the minimal cost condition is called "optimization." The acceptable cost to reduce the collective dose to a population of exposed persons falls within a range of $500 to $2,500 per personrem21 [1 rem = 10 mSv]. The collective effective dose from dental radiographic procedures is presently estimated to be 0.004 mSv/yr. The expenditure of $500 to $2,500 to reduce the collective dose that is presently 735X lower than annual background radiation levels; and 2,500X lower than the 10 mSv collective dose reduction goal is clearly unjustifiable by the imaginary and immeasurable gain in potential benefit.
NCRP Report No. 145 emphasizes the desirability of incorporating a more consistent and strict application of radiographic selection criteria and the incorporation of certain quality assurance procedures, the use of faster image receptors, timetemperature processing, proper interpretation strategies. Such recommendations have merit and certainly deserve appropriate consideration for incorporation into the practice to reduce patient exposures and maintain the highest diagnostic quality radiographs.
Conclusions:
This paper attempts to analyze some of the factual information presented in NCRP Report No. 145, and compares this data in ways that clearly place the public health and occupational risks associated with dental radiography into a clear perspective through comparison of the reported doses attributable to patient and occupational exposures in dentistry with current dose limits and background radiation. In every instance, the effective dose to patients and occupational exposures are many, many times lower than background or the relevant dose limits governing occupational and public exposure. This paper also discusses specific recommendations from Report No. 145 which appear to lack credible supporting evidence, or a significant failure to perceive the impact of their own recommendation; examples include fluoroscopy of lead aprons annually and the specification that rectangular collimated beams not exceed source to image receptor distances by 2% resulting in the potential to have a separate BID or rectangular beam collimating film holder set for each image receptor size in use.
There are several positive benefits to be derived from incorporating some of the reports recommendations into dental radiography practices that should be emphasized. The consistent application of radiographic selection criteria in the prescription of radiographic examinations, the use of faster image receptors and screen/film combinations, along with closer attention to principles of radiographic quality assurance will provide dentists with high quality diagnostic images along with reduced patient dose.
Data provided in Report No. 145 is used as evidence to indicate that dental radiography in the U.S. is already ALARA and that the expenditure of additional financial resources to achieve an even greater level of ALARA is probably unjustified and unmerited since present risks are already immeasurable, undetectable and do not jeopardize the public health. Indeed, two previous NCRP reports have already drawn this conclusion: NCRP Report 107: "It is tempting to conclude that further occupational exposure reduction in dentistry may not be cost-effective." NCRP Report 93 recognizes the "trivial" nature of the dental effective dose equivalent in contributing to calculating a collective effective dose equivalent by stating: "Dental examinations have been omitted since they are estimated to contribute less than 0.01 mSv (1 mrem) to the total average annual effective dose equivalent."
The scientific principle used to under gird NCRP Report No. 145 is the assumption that radiation risks may be extrapolated indefinitely in a linear fashion from high doses to very low doses, the linear nonthreshold theory [LNT]. Polycove15 cites Dr. L.S. Taylor, past president of the National Council on Radiation Protection, as describing the linear extrapolation from high doses to very low doses in the calculation of collective doses as: "deeply immoral uses of our scientific heritage" [p366]. Bond, et al22 writing in opposition to the LNT: "The above arguments also appear to have destroyed rather completely the interpretations of and impressions from the linear hypothesis - that 'low level' irradiation should be of major personal or public health concern, a factor that has induced an almost pathological fear of low level irradiation in a major segment of the general population...It appears to be more sophistry than science, and reminiscent of the 'angels on the head of a pin' debates, to argue about whether a small amount of radiation energy can cause an excess malignancy... one excess cancer can not affect significantly a public health problem of the magnitude of cancer." Additionally, Kellerer and Nekolla22 appear to make a plea for a common sense approach to low dose radiation risk estimation when they state: "There is however, less agreement on the potential health effects of small doses. Such effects cannot be assessed in epidemiological investigations, nor can they be reliably inferred from cell studies or animal experiments... Speculative as such unobservable phenomena are, they cannot be ruled out - but common sense can ignore them." Abel Gonzalez23, as recently as Sept. 2004 has stated: "For purposes of radiation protection, however, the non-threshold concept at doses below background doses is not relevant. It is applicable only for doses above the prevalent background dose that is unavoidably incurred... Therefore, the discussion on whether smaller absolute dose, say some microsievert per year, would be able to induce health effects, or whether the dose-response relationship is LNT at such small doses is an interesting academic question but meaningless for practical radiation protection purposes."
Finally, NCRP Report No. 145 represents an "advisory opinion" on minimizing radiation risks to patients, the dentist and dental staff from dental diagnostic radiographic procedures. NCRP Reports are frequently used by various federal and state entities to establish rules and regulations; as a result it is critically important for dentists and dental x-ray technicians to understand what the NCRP has recommended for the practice of dental radiography because many of the 109 recommendations could, in the near future, become regulations and laws. Report No. 145 clearly places each dentist and x-ray technician, laboratory at a crossroad for decision-making. Every dentist and dental x-ray laboratory is encouraged to obtain a copy of the report and along with the information presented in this paper decide to either support, or not support, the incorporation of Report No. 145's many recommendations into State, Federal, OSHA, EPA and DOE regulations governing the practice of dental radiography. If you support the document's recommendations, then work actively for their incorporation into your State's practice act. On the other hand, if you do not support incorporating some or all of the recommendations in your State, then be vigilant and work with your legislative and State Board representatives and public health officials to see that they are not incorporated into the rules and regulations governing the practice of dental radiography. A failure to act on your convictions will permit someone else to decide how you will practice dental radiography in the future. The choice is ours.
REFERENCES
- NCRP Report No. 145, Radiation Protection in Dentistry. 2003, National Council on Radiation Protection and Measurement, 7910 Woodmont Ave., Suite 400, Bethesda, MD.
- NCRP Report No. 35, Radiation Protection in Dentistry. 1970, National Council on Radiation Protection and Measurement, 7910 Woodmont Ave., Suite 400, Bethesda, MD.
- NCRP Report No. 107, Implementation of the Principle of As Low As Reasonably Achievable [ALARA] for Medical and Dental Personnel. 1990, National Council on Radiation Protection and Measurement, 7910 Woodmont Ave., Suite 400, Bethesda, MD.
- NCRP Report No. 121, Principles and application of collective dose in radiation protection. 1995: 45, National Council on Radiation Protection and Measurements, Bethesda, MD.
- Langland, OE, Langlais, RP, Preece, JW. Principles of Dental Imaging, 2nd ed. Lippincott Williams & Wilkins; 2002:45.
- NCRP Report No. 91, Recommendations on limits for exposure to ionizing radiation. 1987. National Council on Radiation Protection and Measurements, Bethesda, MD.
- NCRP Report No. 93, Ionizing radiation exposure of the population of the United States. 1997, National Council on Radiation Protection and Measurements, Bethesda, MD.
- Graham S, Levin ML, Lilienfeld AM, et al. Preconception, intrauterine, and postnatal irradiation as related to leukemia. National Cancer Institute Monograph, 1966; 19:347-71.
- Preston-Martin S, Thomas DC, White SC, Cohen D. Prior exposure to medical and dental x-rays related to tumors of the parotid gland. J Natl. Cancer Inst. 1988; 80:943-9.
- Preston-Martin S, White SC. "Brain and salivary gland tumors related to prior dental radiography: implications for current practice." JADA 1990; 120:151-8.
- Billen D. Spontaneous DNA damage and its significance for the 'Negligible Dose' controversy in radiation protection. Rad. Res. 1990; 124:242-5.
- Bennett BG. Exposures to natural radiation worldwide, in: Wei L, Sugahara T, Tao Z, editors, High Levels of Natural Radiation 1996 Radiation Dose and Health Effects. Elsevier, Amsterdam; 1997:16.
- Kesavan PC. Indian research on high levels of natural radiation: pertinent observations for further studies, in: Wei L, Sugahara T, Tao Z, editors, High Levels of Natural Radiation 1996 Radiation Dose and Health Effects. Elsevier, Amsterdam. 1997: 112-7.
- Ghiassi-nejad M, Mortazavi SMJ, Cameron JR, Niroomand-rad A, Karam PA. Very high background radiation areas of Ramsar, Iran: preliminary biological studies. Health Physics, 2002; 82:87-93.
- Polycove M. Nonlinearity of Radiation Health Effects, Environmental Health Perspectives 1998. 1998; 106 [Suppl.1]: 363-8.
- Hofmann W, Katz R. Track structure analysis of radiation carcinogenesis at low doses, in: Booz J, Ebert, HG, editors; 8th Symposium on Microdosimetry, Harwood Acad. Pub. EUR 8395. 1983; 565-73.
- Walinder G. Epistemological problems in assessing cancer risks at low radiation doses. Health Phys. 1987; 52:675-8.
- Trosko JE. "Role of low-level ionizing radiation in multi-step carcinogenic process." Health Phys. 1996;70:812-22
- ADA Survey Center's "Distribution of Dentists in the United States By Region and State, 2001" - American Dental Association, 211 E. Chicago Ave., Chicago, IL.
- DOE STANDARD - Applying the ALARA process for radiation protection of the public and environmental compliance with 10 CFR Part 834 and DOE 5400.5 ALARA Program Requirements, Volume 1. U.S. DOE, Washington, DC. 1997
- LLNL Occupational Radiation and Protection Program, Environment, Safety & Health Manual, "ALARA Design Criteria", Document 20.4. http://www.llnl.gov Accessed Aug. 12, 2004.
- Keller AM, Nekolla EA. The LNT-Controversy and the concept of 'Controllable Dose.' Health Phys. 2000; 79: 412-8.
- Gonzalez, AJ. Radiation Safety Standards and their application: International policies and current issues. Health Phys. 2004;87: 258-72.